NCS Journal Club Round-Up #NCSTJC: November 2023
Published on: April 23, 2024
Moderators: @labic6, @twmagnus, @gdomeni
Link to Twitter Thread: https://twitter.com/neurocritical/status/1724443564413772119
The November Neurocritical Care Society Twitter Journal Club featured a discussion on the article “Current Practices for ICP & Cerebral Oxygenation Monitoring in Severe TBI: A Latin American Survey” by Godoy et el. The Latin America Brain Injury Consortium (LABIC) conducted an anonymous survey to understand current practices in Latin America about ICP and brain oxygen monitoring in severe TBI (sTBI). A total of 596 responses from 18 countries were received. Fifty-four percent of the respondents worked in public hospitals and 31% worked in private institutions. Of the institutions, 13.5% were university affiliated. Eighty-two percent of the ICUs were polyvalent, whereas 9% were neuro-intensive care units. Of the respondents, 43.5% reported managing between 25 and 75 patients with sTBI per year.
A broad discussion on the article was held on Twitter (X) for the #NCSTJC with questions in both English and Spanish, and below we review the topics and opinions expressed by participants. We have compiled and translated the responses in both languages.
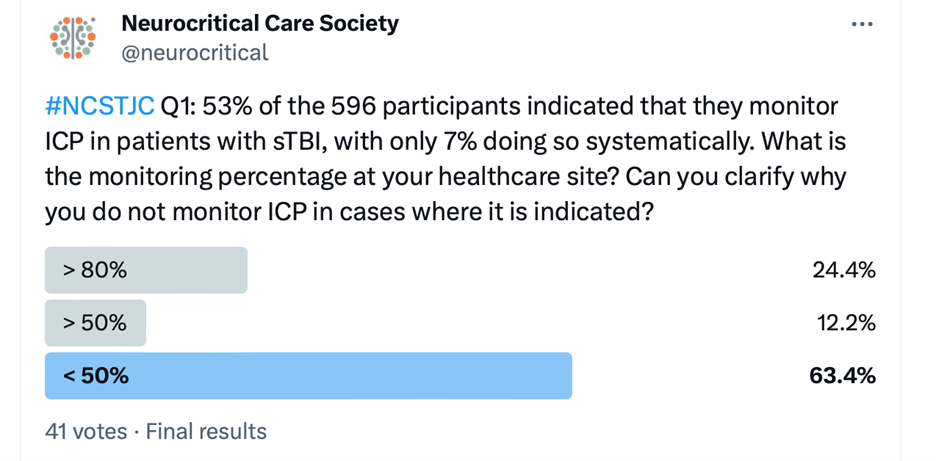
In response to the question about monitoring intracranial pressure (ICP) in patients with severe traumatic brain injury (sTBI), 24.4% monitored in >80%, 12.2% monitored 50%, and 63.4% monitored <50%. Notably, @gdomeni explained in low-income countries, a lack of resources often drives the decision to not systematically monitor ICP. @TJUHNeuroCrit linked to two separate studies on ICP monitoring. The first (https://pubmed.ncbi.nlm.nih.gov/31203067/) demonstrated an unclear benefit of ICP monitoring in improving care for severe TBI patients, leading to a significant decline in its use after 2014. The second (https://pubmed.ncbi.nlm.nih.gov/31954892/) showed that despite lower utilization of ICP monitoring in Pennsylvania since 2014, ICP-monitored patients had a lower risk of in-hospital mortality.
@tchaaban1 highlighted barriers to ICP monitoring, including lack of neurosurgeon buy-in, perceived poor prognosis, and randomized controlled trials (RCTs) not finding a benefit. @dr_mcpato referred to research (https://www.nejm.org/doi/full/10.1056/nejmoa1207363) specifically mentioning the BEST TRIP trial, which demonstrated that protocolized management of head trauma can compensate for resource limitations, leading to the CREVICE protocol (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7249475/).
In response to @dr_mcpato's suggestion, @samednc2022 agreed and proposed moving towards complementary non-invasive monitoring, a "CREVICE plus." @gdomeni questioned the type of monitor proposed, and @dr_mcpato suggested using optic nerve sheath and transcranial doppler for ICP calculation, and jugular bulb and regional oxygen saturation for PbtO2 approximation.
This discussion reflects a diverse range of perspectives on ICP monitoring, including challenges in resource-limited settings, conflicting study findings, and potential advancements towards non-invasive monitoring methods.
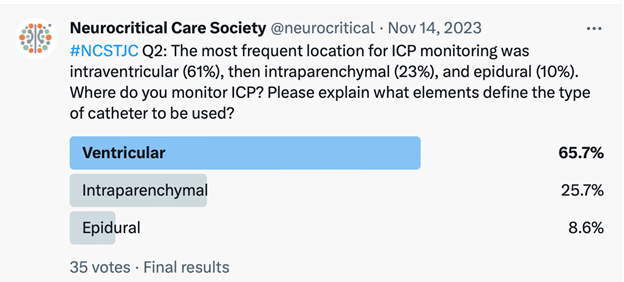
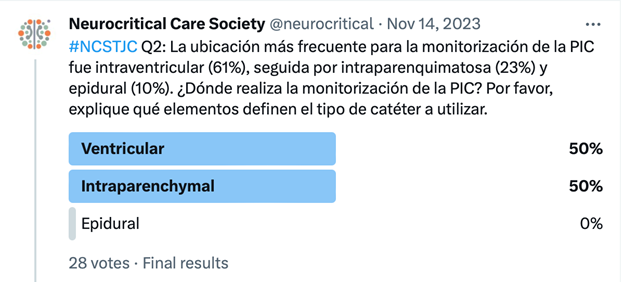
Question 2 featured a poll asking participants about their ICP monitoring practices. Discussion was started by, @dr_mcpato who expressed a preference for intraventricular ICP monitoring. Meanwhile, @samednc2022 discussed various factors influencing the choice of ICP monitoring, including ventricular size, surgeon's experience, patient age, monitoring system availability, and the critical consideration of ventricular catheter infection. In response to @gdomeni's question about non-surgical physicians learning these techniques in resource-scarce settings, @samednc2022 clarified that while ventricular catheter placement should be performed by a neurosurgeon, intraparenchymal catheters could be installed by non-surgeon specialists with proper training. This led to further discussions on the nature of proper training and considerations for expanding training within local policies, with @keatonSmetan sharing a publication (https://link.springer.com/article/10.1007/s12028-018-0556-2) suggesting the effectiveness of non-neurosurgeon professionals in placing external ventricular drains.
@gabeknowz added insights about pathology, ventricular anatomy, and local neurosurgeons often driving decisions. @CanrillMauricio stated intraventricular is the preferred, but intraparenchymal locations being more common in their practice.
In the survey, a mere 14.6% of respondents reported monitoring cerebral oxygenation, and an even smaller 2.2% monitored brain tissue oxygen pressure. This prompted the question of whether economic limitations are a hindrance to such monitoring practices and if they indeed influence the management of brain injuries. @CantillMauricio asserted that economic constraints are a harsh reality, emphasizing the need to persuade hospital authorities for support. @twmagnus chimed in, highlighting the vast cost differences between devices for intraparenchymal oxygen monitoring compared to SjO2 or intraventricular pressure monitoring. @gdomeni added a layer to the discussion, noting that the monitoring of oxygenation is constrained by both resource scarcity and a limited understanding of its utility. Furthermore, stated that the definitive benefits of brain tissue oxygen pressure monitoring remain unclear, as indicated by the reference (https://pubmed.ncbi.nlm.nih.gov/37863590/).

The discussion on barriers to neuromonitoring encompasses various perspectives. @gdomeni emphasized the lack of understanding of the positive impact of monitoring as a significant barrier, in addition to challenges related to financial support, knowledge of techniques, and proper use. @ChristosLazari3 questioned the strength of evidence for ICP monitoring and @gdomeni suggested a shift in focus towards discussing how to guide accuracy for individual patients. @DrRibCM offered a cautious perspective on generalizing from surveys, stressing the importance of real and reliable data. @twmagnus identified barriers such as the unavailability of authorized distributors in Latin American countries, neurosurgeons’ reluctance toward invasive monitoring, and a lack of understanding of local policies. @KeatonSmetana emphasized the need to understand practice variations for personalized medicine under global resource constraints. @CantillMauricio highlighted the economic situation in Latin America as a primary barrier and stressed collaboration with supportive neurosurgeons.
In response to the question on whether personalized management guided by neuromonitoring enhances the effectiveness of severe traumatic brain injury (sTBI) care, @gdomeni underscored the key factor is personalized management guided by the unique pathophysiology, which varies between patients and injury mechanisms. The crucial consideration is determining the most appropriate neuromonitoring method and the optimal timing in its evolution, posing questions about invasiveness, non-invasiveness, and the data guiding these decisions. @samednc2022 strongly supported the idea that neuromonitoring undoubtedly contributes to more efficient, rational, and individualized patient management in the context of sTBI.
Link to Spanish version