Part 2: Story of Hope – Life After Cardiac Arrest
Published on: September 04, 2024
Ron had to remain intubated for a couple more days while his ventilator settings were weaned. The biggest concern was that he may need to be reintubated if he was extubated too soon, which could result in trauma to his airway. Finally, on day 11, his ICU team felt comfortable removing the breathing tube. He could barely speak above a whisper, but he could talk—and it was clear that he was experiencing severe delirium as he began to answer the questions posed by his nurses and doctors.
Despite receiving reminders every shift, he was unable to retain the information given to him regarding why he was in the hospital and how long he’d been there. Over and over again he’d say that we had to leave: “We gotta get out of here.” But I knew there was no chance of him leaving AMA—or "against medical advice”—in my absence, because he had become so weak he wasn’t even able to roll over in bed by himself, much less walk out of the hospital. He was very confused, and it was clear he would need extensive physical, occupational, and speech therapy as part of his recovery.
***
During this time, we had a wonderful nurse named Taryn who strongly advised me to advocate for Ron to be transferred to Strong’s in-hospital rehab unit on the 5th floor once he was medically ready. He’d receive intensive PT, OT, and speech therapy there for several hours per day, and it would set him up for the best possible cognitive and physical outcome. The only issue would be getting him to the point where he could tolerate it, as he remained medically unstable with frequent bouts of low blood pressure, and he was still unable to get out of bed or bear weight.
Finally, after 12 days in the ICU, we received word that Ron was stable to be transferred to a medical unit that day. His nurses and doctors described his recovery since waking up as “miraculous,” saying “we never see this outcome.” They let me know that it was quite rare for a patient who’d been as sick as Ron to be able to transfer straight to a medical floor from the ICU without first needing step-down care. Despite his improvements, Ron was still receiving nutrition from a feeding tube and was unable to get out of bed. He was also still in a state of severe delirium and would need quite a bit of supervision, but he no longer required the higher complexity of care of an ICU patient. Coming out of the ICU also meant that he’d have a better chance of recovering from his delirium without all the overstimulation that comes from being in an ICU setting.
never see this outcome.” They let me know that it was quite rare for a patient who’d been as sick as Ron to be able to transfer straight to a medical floor from the ICU without first needing step-down care. Despite his improvements, Ron was still receiving nutrition from a feeding tube and was unable to get out of bed. He was also still in a state of severe delirium and would need quite a bit of supervision, but he no longer required the higher complexity of care of an ICU patient. Coming out of the ICU also meant that he’d have a better chance of recovering from his delirium without all the overstimulation that comes from being in an ICU setting.
After the initial excitement from transitioning out of the ICU, we realized there was still quite a long road ahead and that it was filled with challenges. Ron’s delirium persisted and it was unclear if he would need a gastrostomy tube for longer-term nutrition. Luckily, he was cleared to safely swallow and eat after a few weeks of speech therapy, while the first steps in his cardiac workup had been completed in the meantime—all of which meant he was ready for the next stage of his recovery.
***
Ron was finally transferred to Strong Memorial Hospital’s rehab unit on December 12. During his 23-day stay at the acute brain injury rehab unit, he participated in six hours of therapy every day, and by afternoon he’d fall into bed exhausted. He initially struggled in speech therapy to write his name, remember numbers, complete simple brain puzzles, and draw a picture. He would tire in OT at first, resting his head in his hands during tasks, and his blood pressure would often drop during physical activity, so he’d need to wear a binder and compression socks to prevent it from happening during PT and make it through his sessions. Despite all of this, he pushed through and began to get stronger by the day. He went from using a walker and a gait belt to walking without an assistive device, and soon began to complete his tasks in OT with ease. We were hopeful, and as time went on, saw that he would without a doubt be ready for discharge home on his target date of January 4, 2023. His doctors told us that he should continue to improve at home until he reached about one year post-arrest.
As in the ICU, we bonded with the wonderful staff during Ron’s stay in the rehab unit, and one of our favorite nurses was Carol, whose humor always set the tone for the day. Carol brought an alarm clock in for Ron because he had his days and nights mixed up, and always stopped in his room to visit and joke with him whether he was her patient that day or not. She made sure to say goodbye on the day of our discharge home, and she brought plenty of cookies and hugs too. By that point, we couldn’t believe the day had finally come that Ron was going home.

Ron’s arrival home on January 4, 2023. Ron has his arm around Becky Kane, the deputy who was first to respond to the 911 call. To Ron’s left is Billy Boyd, the 911 dispatcher who took the initial call.
***
I would love to say that it was smooth sailing from there on, but once we got past the initial elation of Ron cheating death, we realized that our work had only just begun. The first months at home were a struggle. Ron came home on twenty medications. He’d been diagnosed in the hospital with severe central sleep apnea, likely brought on by his cardiomyopathy, and needed to use a CPAP machine. He continued to receive PT, OT and speech therapy six times per week at home. He had regular follow-up appointments with Cardiology, Cardiac Electrophysiology (EP), Neurology, Physical Medicine and Rehabilitation, Sleep Medicine, and his primary care physician. His body was still weak, having lost thirty pounds in the hospital, and he took a few falls. He suffered from nausea and intestinal upset. His days and nights were still flipped, and at times, he’d awaken for the day at 3 a.m.
Gradually, though, as Ron applied his lifelong work ethic to his recovery process, his in-home PT, OT and speech therapy were moved over to an outpatient setting, and he finally graduated from all therapies by September 2023. Today, his only remaining specialist is Dr. Xiao, his Cardiologist, whom he’ll continue to see once every year. At Ron’s last visit in November, Dr. Xiao said that his repeat echocardiogram showed that his heart had repaired itself completely, and his ejection fraction had risen from 21% post-arrest to 55%. Along with the improvement of Ron’s cardiac function, his sleep apnea has also spontaneously resolved. But perhaps one of his greatest accomplishments in Ron’s own eyes is that on November 18, 2023, he returned to “full and strenuous duty” as a Livingston County Sheriff’s Deputy.
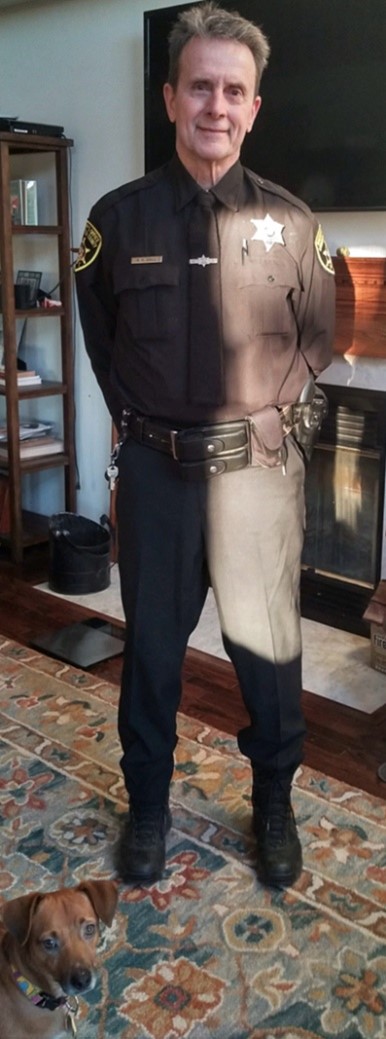
Ron on his first day back to work as a Sheriff’s Deputy
We could not have made it through Ron’s illness and recovery period without the love and support of so many family members and medical staff. The most vivid memories Ron has of his time in the hospital are of his wonderful nurses and doctors. And we’ve been fortunate enough to have the most loving, steadfastly supportive family members and friends in our lives. We feel like the luckiest people in the world—because we are.