Glen’s Story of Hope
Published on: June 16, 2025
After landing in Atlanta on August 1, 2023, Glen Schultz made his way to the Sky Lounge at Hartsfield Jackson Airport to ride out his layover and check in with his family, as was his routine during his work trips. Glen had been en route to South Carolina following a speaking engagement in Alabama. In addition to being a three-time author and professor, he is founder and director of Kingdom Education Ministries, an organization developed for the purpose of educating future leaders to think and act from a biblical worldview. He has been married to his wife Sharon for 55 years and has three children and six grandchildren.
|
|
While in the lounge, Glen called his son, Jason, who was on vacation in Montana. On that call, Jason noticed that Glen, who was a proficient public speaker even at 76 years old, was slurring his words and speaking in incoherent sentences. Jason knew immediately that something was wrong and spent the next 45 minutes trying to contact emergency services in Georgia. Glen’s grandchildren got on the phone to keep him occupied while Jason attempted to do the impossible and get Atlanta EMS to find Glen in one of many lounges in the busiest airport in the world. This initiated a cascade of events that eventually got Glen transported to Grady Memorial Hospital.
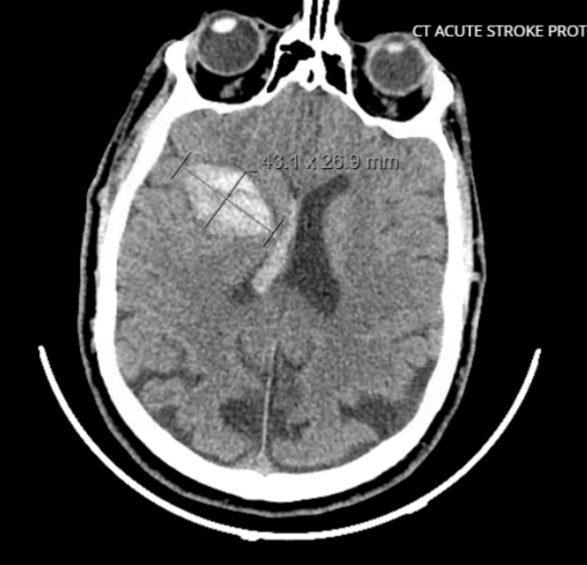
When he arrived in the emergency room at Grady, he was vomiting and no longer able to breathe safely. This prompted the emergency room physicians to place a breathing tube and put Glen on a ventilator. Unfortunately, a CT scan of his head showed a hemorrhage on the right side of his brain. With no history of hypertension and normal blood pressure upon arrival to the hospital, Glen’s physicians determined that his brain bleed was most likely due to cerebral amyloid angiopathy (CAA), a condition where abnormal amyloid proteins build up and cause damage in blood vessels in the brain.
Glen’s neurologic function improved from his early unresponsiveness, although he had many of the manifestations expected from a right-sided brain injury, such as left-sided weakness. Still, he maintained an extraordinary ability to communicate via writing. During morning rounds, he could be seen from the hallways paying his bills and writing instructions to his wife Sharon on how to handle their business affairs.
His stay in the ICU was a rollercoaster of ups and downs. His neurosurgery team placed a drain to help relieve the pressure that was building up in his brain, but the team would have a tough time getting it out in the ensuing days, as Glen continued to rely on the drain to maintain normal intracranial pressures. He also developed pneumonia, which is a common complication for patients supported by ventilators. After a little more than a week of these ups and downs, Glen and his family were advised to start thinking about planning for a tracheostomy and gastrostomy tube placement. These procedures would move the breathing tube from his mouth to his neck and allow for his nutrition to go directly through a tube in his stomach—both of which are typically more comfortable for people as they recover from a brain injury.


Considering Glen’s ability to comprehend and express himself, he was naturally invited to participate in the conversations regarding the recommended procedures. When he was asked for his thoughts eleven days after his hemorrhage, Glen wrote fervently, “take the tubes out” and “DNR,” which he underlined three times for emphasis. DNR is a code status that means “do not resuscitate” and would mean the team would not intervene if Glen’s tubes came out and he required further life support. The ICU attending physician explained that taking the tubes out could lead to his death. In response, Glen wrote, “I understand the dangers.” He signed his name to confirm. Sharon looked at us with wide eyes, seemingly pleading with us not to use these words as proof of his actual wishes.
|

|
Over the course of the next few days, Glen had lengthy discussions with his family. He remembers waking up one morning after a long night of prayer with an overwhelming sense of peace and purpose. He had undeniable clarity that his work in this life was not done, and he knew what he had to do. Ultimately, Glen decided to undergo the tracheostomy and gastrostomy tube placement.
After he was discharged to a long-term acute care (LTAC) facility on August 17th, 2023, he spent the next four months transferring from one LTAC to another and then to rehab. With each transfer he inched closer to South Carolina. Finally, on January 11, 2024, he arrived home, over five months from the day he was initially admitted to Grady.
***
I recently called Sharon to get an update. I fully expected her to still be reading Glen’s scribbled thoughts and requests. “Hold on, I have a surprise for you,” she excitedly whispered into the phone. I heard a muffled “Glen, it’s Liz from Grady,” and the next words I heard were his, strong and clear: “Thank you for saving my life.”
Despite our collective perceptions of Glen’s comprehension during his ICU stay, he says his memories are sparse—only foggy memories of a “man in a white coat” but very little else. He described the months spent at LTACs and rehab and all the improvements he had made, now reaching the point of being able to “make the gym” once a day. Outside of getting his reps in, Glen has dedicated himself to the education and support of neurological injury survivors, and he has established a support group at his church.
Glen told me that his faith is what got him through those long, grueling months, and he wanted me to pass along his message of hope, reminding all of us and our patients that anyone can beat the odds. He reflected on attaining peace by knowing that his purpose in this life wasn’t over, and he is now in the midst of writing his fourth book—his own survival story.
