Traumatic Brain Injury in a Resource-Limited Setting: A Reflection on the Importance of Timely Interventions in Neurocritical Care
Published on: May 17, 2024
I work as a physician in the emergency room of one of the busiest hospitals in the Dominican Republic, which also functions as an international referral center. I was just about to finish an especially long shift after having completed what I thought was my last patient evaluation. Suddenly, the emergency room doors burst open, accompanied by the frantic screams of family members and emergency medical technicians urgently seeking directions for where to place the patient they were transporting.
The patient, a 28-year-old male, had crashed into a lamppost. At the scene, 911 was called, but the responding unit, typically staffed by a driver without medical training, lacked adequate medical supplies. Often this is their first job in the medical field and these providers might carry basic medications but usually have no access to oxygen, defibrillators, or airway management equipment.
Initially taken to the nearest public emergency room, the patient was administered mannitol and a saline bolus through two large-bore IVs. However, his condition deteriorated quickly; his oxygen levels fell, and his hemodynamic stability worsened. His family, deeply concerned, insisted on transferring him to a larger medical center about 20 minutes away, a drive lengthened by late-night rush hour traffic.
Upon arrival, I assessed the critically ill patient, who was unable to protect his airway and had not been intubated. His oxygen saturation was perilously low in the 40s. Immediate intubation was attempted but proved challenging due to active bleeding in the upper airway. Despite these challenges, the medical team successfully secured the airway. The patient soon went into cardiac arrest due to hypoxia and hypotension, and after 35 minutes of CPR, spontaneous circulation was restored.
The team then stabilized his condition and performed a CT scan of the entire body, which revealed a large left pneumothorax, a small amount of free fluid in the abdomen, diffuse cerebral edema, and traumatic subarachnoid hemorrhage (Figure 1). A chest tube was inserted on the left side, and the patient underwent an exploratory laparotomy, where a damaged spleen was removed. He was then transferred to the intensive care unit.
By the second day, the patient displayed clinical signs of intracranial hypertension, including anisocoria and bradycardia with elevated blood pressure — symptoms of Cushing’s triad. An urgent CT scan showed worsening cerebral edema and right temporal and bi-frontal contusions (Figure 2). A decompressive craniectomy was performed, but malignant edema continued with excessive transcalvarial herniation and midline shift (Figure 3). Despite all efforts and optimizing medical management, the patient's condition declined neurologically until he was declared brain dead through a neurological examination, an apnea test, and transcranial doppler methods.
Figure 1. Initial computed tomography of the head
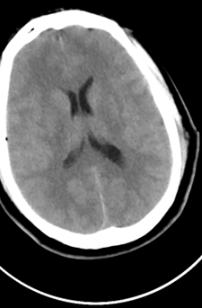
Figure 2. Computed tomography of the head on the second day of hospitalization showing worsening cerebral edema and multifocal contusions (red arrow)
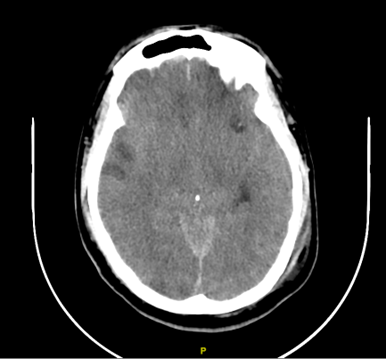

Figure 3. Computed tomography of the head showing worsening cerebral edema with effacement of gray/white matter differentiation, worsening midline shift, and transcalvarial herniation.


Commentary:
The case presented here of a young man who succumbed to what could have been a survivable brain injury highlights systemic issues in the Dominican Republic, where motor vehicle accidents are the leading cause of death, much like in many other low- and middle-income countries (LMICs). This tragic event underscores the critical need for improved on-scene airway management and resuscitation efforts.
Traffic injuries are a global issue, but their impact is disproportionately severe in LMICs. In fact, LMICs account for about 85% of global traffic injury fatalities.1 In cases like this one, immediate administration of supplemental oxygen is recommended for all patients with suspicion of moderate or severe TBI, regardless of their baseline oxygen saturation.2 Indeed, TBI management begins at the scene of the injury, emphasizing the importance of resuscitation and preventing secondary insults caused by hypotension (by maintaining SBP > 110) and hypoxia (maintaining SatO2 > 90%).2
However, adopting best practices for pre-hospital care is challenging in resource-limited settings like the Dominican Republic in comparison to higher-income countries. A systematic literature review showed significant challenges in pre-hospital care across various LMICs.3 Poor infrastructure, including road access, inadequate availability of basic materials, and a lack of coordination and fragmented systems, were frequently cited as obstacles to the efficient operation of pre-hospital care services.3 As in other countries, members of the public who often lack medical training are the first responders for the majority of patients in these settings, resulting in potential delays in receiving appropriate care. There is a notable lack of standardized protocols for transporting patients to hospitals, with many studies indicating that patients are often transported by family members or private vehicles rather than ambulances. As a result, many patients arrive at definitive trauma centers well beyond the recommended "golden hour" for optimal treatment.1,3 Only a minority of ambulances in LMICs are staffed by physicians or equipped with personnel trained in basic life support.3 These personnel might not fully understand how brain hypoxia triggers cerebral vasodilation through autoregulatory mechanisms, contributing to intracranial hypertension.2 In the case presented, the patient’s severe hypoxia not only contributed to these complications but also led to a cardiac arrest that could have been prevented with more prompt and appropriate medical intervention.
To optimize the management of TBI patients in LMICs, various protocols have been developed to address resource limitations. Among these, a noteworthy protocol named "Beyond One Option for Treatment of Traumatic Brain Injury: A Stratified Protocol (BOOTStraP)" stands out for its inclusion of pre-hospital care.4 This innovative approach offers ten protocols tailored to different resource contexts, ranging from minimal to high levels of resources. Users can select the most suitable treatment option based on available resources and transition to other options as resources fluctuate, reflecting the common challenges faced by practitioners in resource-constrained regions.
However, we may soon gain insights into how to improve pre-hospital care for patients with TBI. The MOTOR trial, a two-armed parallel multiple-period cluster randomized controlled clinical trial, is currently in progress.5 This trial in Ugandan trauma centers aims to assess the impact of a locally adapted rural trauma team development course (developed by the American College of Surgeons) on process and patient outcomes such as morbidity and mortality. The findings of this trial have the potential to inform the design, implementation, and scalability of rural trauma team development programs in similar low-resource settings.
In LMICs, while the prehospital system faces numerous challenges, there are also promising opportunities for enhancement. Collaborative efforts among government agencies, healthcare providers, civil society organizations, and international partners can leverage expertise, resources, and networks to enhance prehospital care in resource-constrained settings. Several studies have highlighted the significant role of community members and non-medical first responders in delivering prehospital care. By involving and empowering communities, there is potential to increase demand for prehospital services and facilitate improvements in their quality and accessibility.6
Dr. Morel is privileged to work in one of the Dominican Republic's most advanced healthcare facilities. However, despite this privilege, there remains a pervasive concern about the significant delays in accessing medical care for oneself or loved ones during emergencies. The reality remains that the actions taken in the initial moments following a TBI are arguably the most critical aspect of the treatment process. Future research will need to focus on adapting rural trauma team training to LMIC settings, aiming to equip traffic law enforcement and medical trainees with essential skills that could establish a new standard for trauma care and educational frameworks in these regions. We are optimistic that the MOTOR trial will illuminate a path forward.
References
- Wan R, Xia J, Duan F, Min L, Liu T. Global burden and trends of transport injuries from 1990 to 2019: an observational trend study. Inj Prev. 2023;29(5):418-424. doi:10.1136/IP-2023-044915
- Hawryluk GWJ, Lulla A, Bell R, et al. Guidelines for Prehospital Management of Traumatic Brain Injury 3rd Edition: Executive Summary. Neurosurgery. 2023;93(6):E159-E169. doi:10.1227/NEU.0000000000002672
- Bhattarai HK, Bhusal S, Barone-Adesi F, Hubloue I. Prehospital Emergency Care in Low- and Middle-Income Countries: A Systematic Review. Prehosp Disaster Med. 2023;38(4):495. doi:10.1017/S1049023X23006088
- Rubiano AM, Vera DS, Montenegro JH, et al. Recommendations of the Colombian Consensus Committee for the Management of Traumatic Brain Injury in Prehospital, Emergency Department, Surgery, and Intensive Care (Beyond One Option for Treatment of Traumatic Brain Injury: A Stratified Protocol [BOOTStraP]). J Neurosci Rural Pract. 2020;11(1):7-22. doi:10.1055/S-0040-1701370
- Lule H, Mugerwa MA, SSebuufu R, et al. Title Effect of rural trauma team development on outcomes of motorcycle related injuries: A protocol for a multi-center cluster randomized controlled clinical trial (The MOTOR trial) Names of protocol contributors. doi:10.1101/2023.12.07.23299662
- Prust ML, Mbonde A, Rubinos C, et al. Providing Neurocritical Care in Resource-Limited Settings: Challenges and Opportunities. Neurocrit Care. 2022;37(2):583-592. doi:10.1007/S12028-022-01568-2