#NCSTJC: November 2024 NCS Twitter Journal Club Round Up
Published on: May 13, 2025

November 2024’s NCSTJC focused on an article published in Neurocritical Care in March 2024 titled “Association Between Early Mobilization and Functional Outcomes in Patients with Aneurysmal Subarachnoid Hemorrhage: A Multicenter Retrospective Propensity Score-Matched Study.” This study examined how early mobilization (within 72 hours) affected functional outcomes in patients with aneurysmal subarachnoid hemorrhage (aSAH). Results showed that early mobilization was linked to better functional outcomes at discharge. November’s journal club was unique as it was co-hosted on LinkedIn in addition to X.

The first prompt of the discussion was a poll asking participants to decide what they believed to be the most significant benefit of early mobilization in the aneurysmal subarachnoid hemorrhage population. While there were varied responses, a slim majority chose “Improved functional independence” as the most significant benefit over “Lower complication rates.” No respondents chose “Shorter hospital stays” and only two chose “Enhanced cognitive recovery.”


The next poll asked respondents which secondary outcome would have the greatest weight to advocate for its use at their own institution. Despite an earlier question showing no respondents who selected shorter hospital stay to be the most significant potential benefit, 42% of respondents to this question selected “shorter overall hospital stay” as the biggest factor to advocate for its local use.
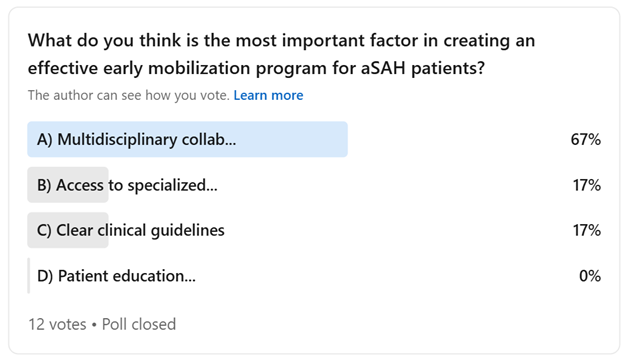
The final question asked participants to select the most important factor in creating an effective early mobilization program for patients with aSAH. The responses were more united on this question with the majority selecting “multidisciplinary collaboration” as the most important factor, while no participants selected “patient education and family support.” Given the need for participation from physical therapists, occupational therapists, respiratory therapists, nurses, advanced practice providers, and physicians as part of a successful early mobilization program, respondents agreed that collaboration is truly key.
In the November edition of the #NCSTJC, which had mostly interactive polling and was cohosted on LinkedIn, participants explored key aspects of the intervention, with half identifying improved functional independence as the primary benefit. Regarding implementation considerations, 42% of participants recognized shorter hospital stays as the most compelling factor for institutional adoption. The discussion highlighted the critical role of multidisciplinary collaboration, with participants emphasizing the importance of coordinated efforts between nursing staff, physical and occupational therapy teams, and respiratory care specialists for successful implementation.
Link to Full Thread: https://www.linkedin.com/posts/neurocritical-care-society_ncstjc-activity-7262119798535331840-wKUY?utm_source=share&utm_medium=member_desktop&rcm=ACoAADhJxxkBa1Jg0wbZJm5m6hZD7P0WAxKDA80