#NCSTJC: May 2024 NCS Twitter Journal Club Round-Up
Published on: September 10, 2024
Moderator: @drdangayach
Link to Twitter Thread: https://x.com/neurocritical/status/1790384213625016369
The May NCSTJC addresses the much-debated topic of hypertonic solution administration in managing cerebral edema. This month’s article is titled “Safety and Effect on Intracranial Pressure of 3% Hypertonic Saline Bolus Via Peripheral Intravenous Catheter for Neurological Emergencies,” published in Neurocritical Care in February 2024. This observational study assessed the incidence of complications with peripherally administered 3% hypertonic saline. The authors found that the complication rates were relatively low, questioning the need for central lines for administration.
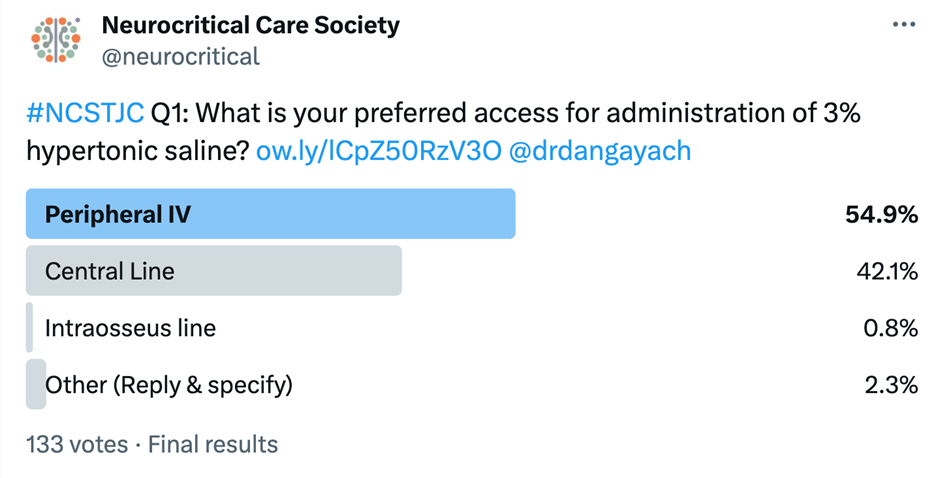
The first question was a poll asking about clinicians’ preferred access for administration of 3% hypertonic saline: 54.9% of respondents chose “peripheral IV,” 42.1% preferred “central line,” 2.3% selected “other,” and 0.8% chose “intraosseous line.” Additionally, @CharlenePringl1 commented: "PIV is fine for a bolus, CVL for infusion (will do 2% through a PIV) if CVL access is an issue." @DCM7200 commented: “There is literally no thought given when it comes to administration of epinephrine pushes in a code. Bolusing HTS should be considered the same. The question is when it’s being run continuously for an arbitrary goal with no exit strategy.”
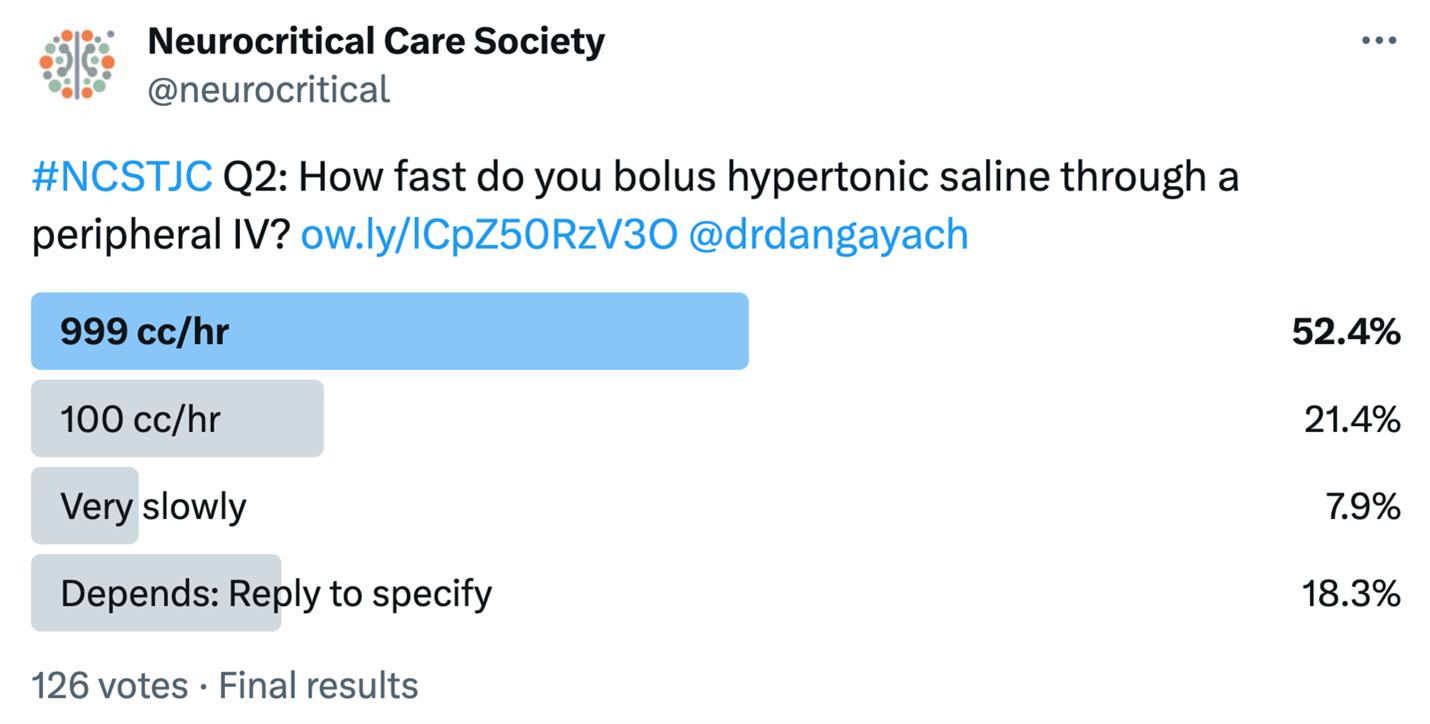
The second question asked how fast clinicians bolus hypertonic saline through a peripheral IV: 52.4% of respondents said “999 cc/hr,” 21.4% said “100 cc/hr,” 7.9% said “very slowly,” and 18.3% responded “it depends” and provided comments. @KeatonSmetana was the first to comment: “Conventional wisdom cautions against solutions >900 mOsm via PIV due to extravasation risks, based on TPN studies over extended periods. However, for acute needs, administering 3% HTS at 999mL/hr =safe + effective. Ideally small bore, large vessel, no flexion area.” @dcm2700 responded: “I would controversially add - administration of HTS for an arbitrary goal or at a high rate for an undefined period of time is nonsensical to me.” Other responses included 75 cc/hr, 20 minutes, and 750 ml/hour.
@EmToxRx added that it can depend on the gauge of the IV and that their biggest issue is that their “bags are 500mL and usual dose we use is 250mL. Especially once you pump up the pressure bag it’s hard to see how much is left.”
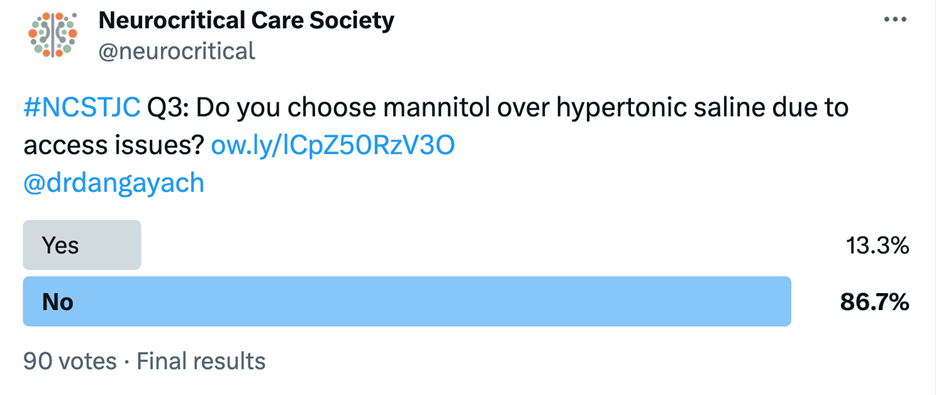
Question 3 asked participants if they preferred mannitol over hypertonic saline due to access issues, with 86.3% replying “no” and 13.3% replying “yes.” @kelseyel_ asked a follow up question: “Curious what concentration mannitol those who voted yes use? Mannitol 20% & 25% both higher osmolarity versus 3% NaCl?” @Drdangayach and @visasht both replied “20%.” While the route and speed of administration of 3% may be up for debate, it is clear participants preferred hypertonic saline over mannitol.
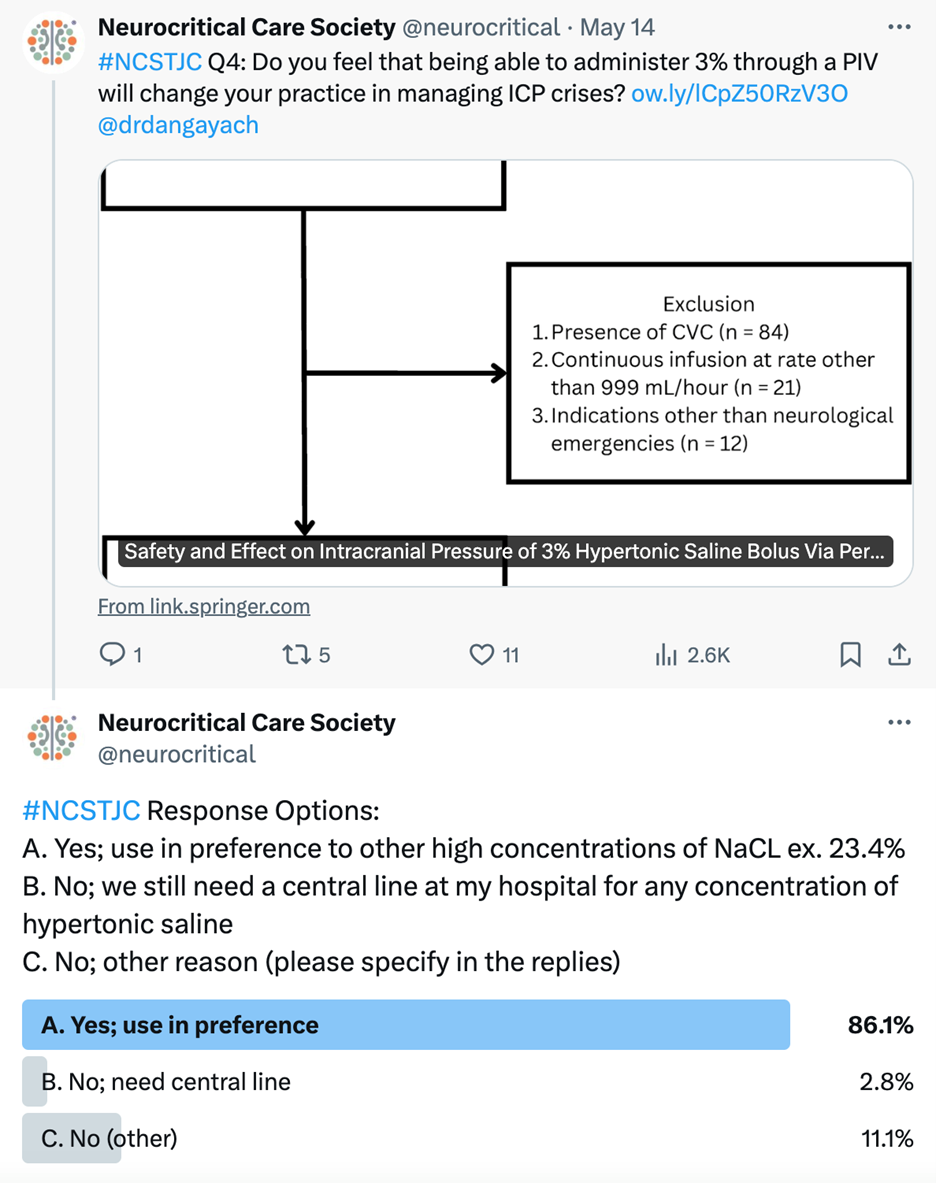
Question 4 asked if the ability to administer 3% hypertonic saline through a peripheral intravenous line (PIV) would change clinicians’ practice in managing intracranial pressure (ICP) crises: 86.1% of respondents said yes (in preference to other high concentrations of NaCl), while 13.9% said no (2.8% because of a continued need for a central line at their hospital for any concentration of hypertonic saline, and 11.1% for other reasons). Overall, most participants agreed that the ability to utilize 3% hypertonic saline peripherally may change their practice patterns.
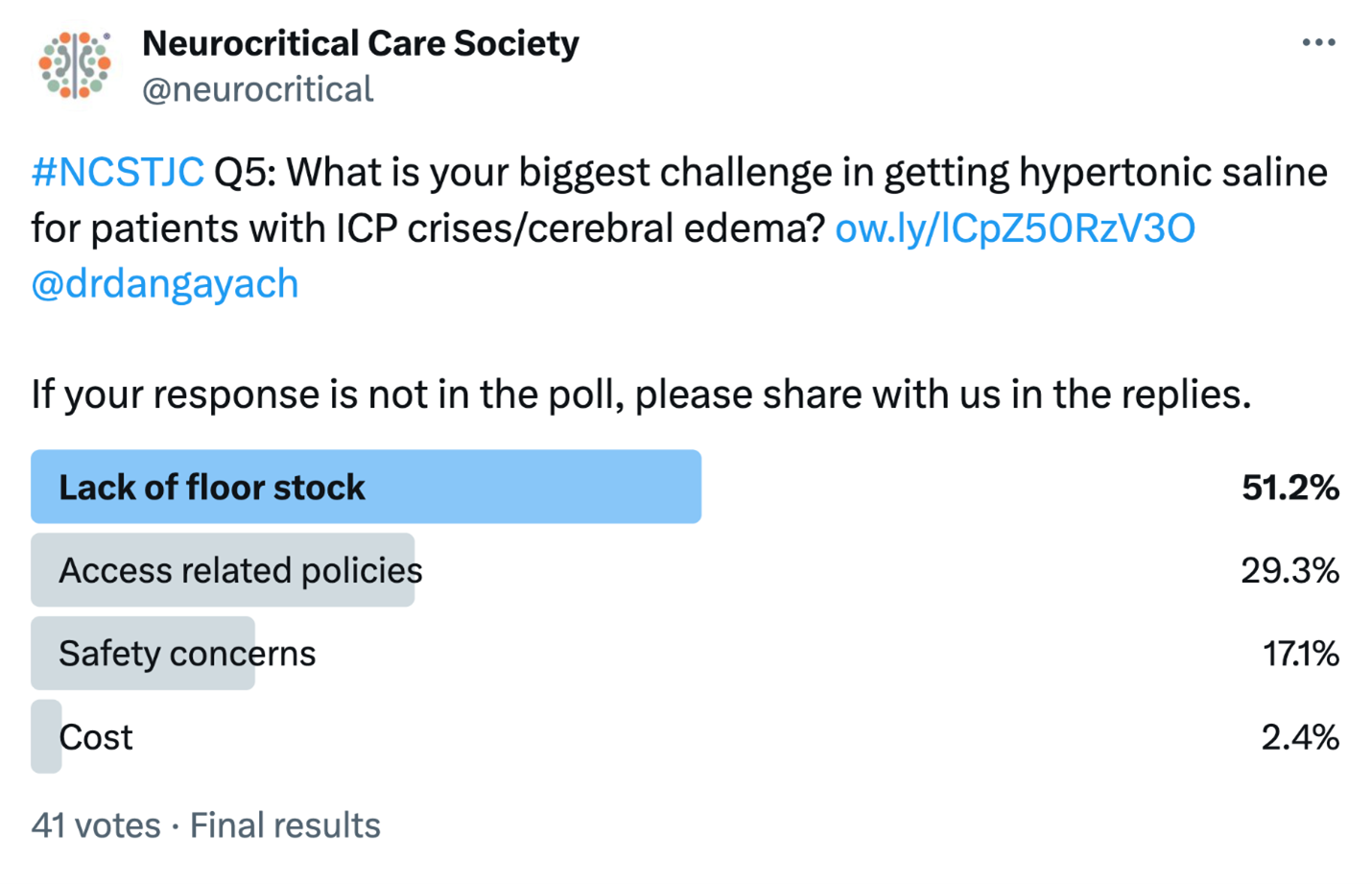
Question 5 asked about the biggest challenges in administering hypertonic saline for patients with ICP crises and cerebral edema: 51.2% of respondents indicated a “lack of floor stock,” 29.3% noted “access-related policies,” 17.1% said “safety concerns,” and 2.4% said “cost.” @KeatonSmetana added that administering hypertonic saline can lead to “hyperchloremic metabolic acidosis, which can be mitigated with sodium acetate / bicarbonate.” For many participants, institutional issues such as policies regarding type of access (peripheral IV versus central line) and ready availability of the medication limits their ability to utilize hypertonic saline.
This week’s NCSTJC featured a thoughtful discussion about the current landscape surrounding the use of hypertonic solutions in treating elevated ICP. It underscored the diversity of practices, as well as institutional guidelines and logistical challenges regarding rapid administration. The potential to administer 3% NaCl peripherally is a major step in addressing these barriers and highlights the increasing evidence supporting the safe and timely use of hypertonic solutions, as well as the research required to overcome other existing obstacles.
Access the article here: https://link.springer.com/article/10.1007/s12028-024-01941-3