#NCSTJC: April 2024 NCS Twitter Journal Club Round-Up
Published on: August 20, 2024
Moderator: @patmchen
Link to Twitter Thread: https://x.com/neurocritical/status/1780960425690935674
April’s #NCSTJC involved a discussion around the article titled “Barriers to Surrogate Application of Patient Values in Medical Decisions in Acute Stroke: Qualitative Study in a Biethnic Community.” This was an intriguing article centered on the difficulty of surrogate decision-making and the different barriers that exist for surrogates of both Mexican-American and non-Hispanic white patients.

@NezerSara was the first to chime in, saying “I am trying to take back the ‘family meeting’ as something we do BEFORE hard decisions have to be made; lay the groundwork early and often on what proxy means.” @patmchen added: “From my experience many never think of possibility of being a proxy decider so need time and many conversations to ‘teach’ what this means.” Both brought up the often-impossible decisions families face and the importance of educating family members on their roles in this decision-making process.

The second question was a poll on when neurocritical care clinicians start addressing the gap in surrogates’ ability to apply a family member’s previous values: 38.9% of respondents said "early," with 44.4% responding “after the first 24-48 hours,” 5.6% responding “at the family meeting,” and 11.1% providing other comments. @rkchoi agreed with “early,” asserting that it is “important to continue to reiterate that family are surrogate decision makers who should uphold the patient’s wishes, not their own, as difficult as that may be.” Moderator @patmchen also agreed, suggesting it should be “much earlier than typical, especially if the injury has a clearly severe trajectory. We expect families to make significant decisions about withdrawal vs trach and peg around day 14 when the concept of deciding from the perspective of another is very foreign.” Overall, participants clearly noted the importance of having early conversations with family to bridge the gaps between patient and family wishes.
@KeatonSmetana responded: “Engage in open dialogue about cultural values, prioritize advance care planning, and offer individualized support to respect the unique perspectives of patient independence and family time.” @patmchen brought up the need for further education for our trainees on this topic.
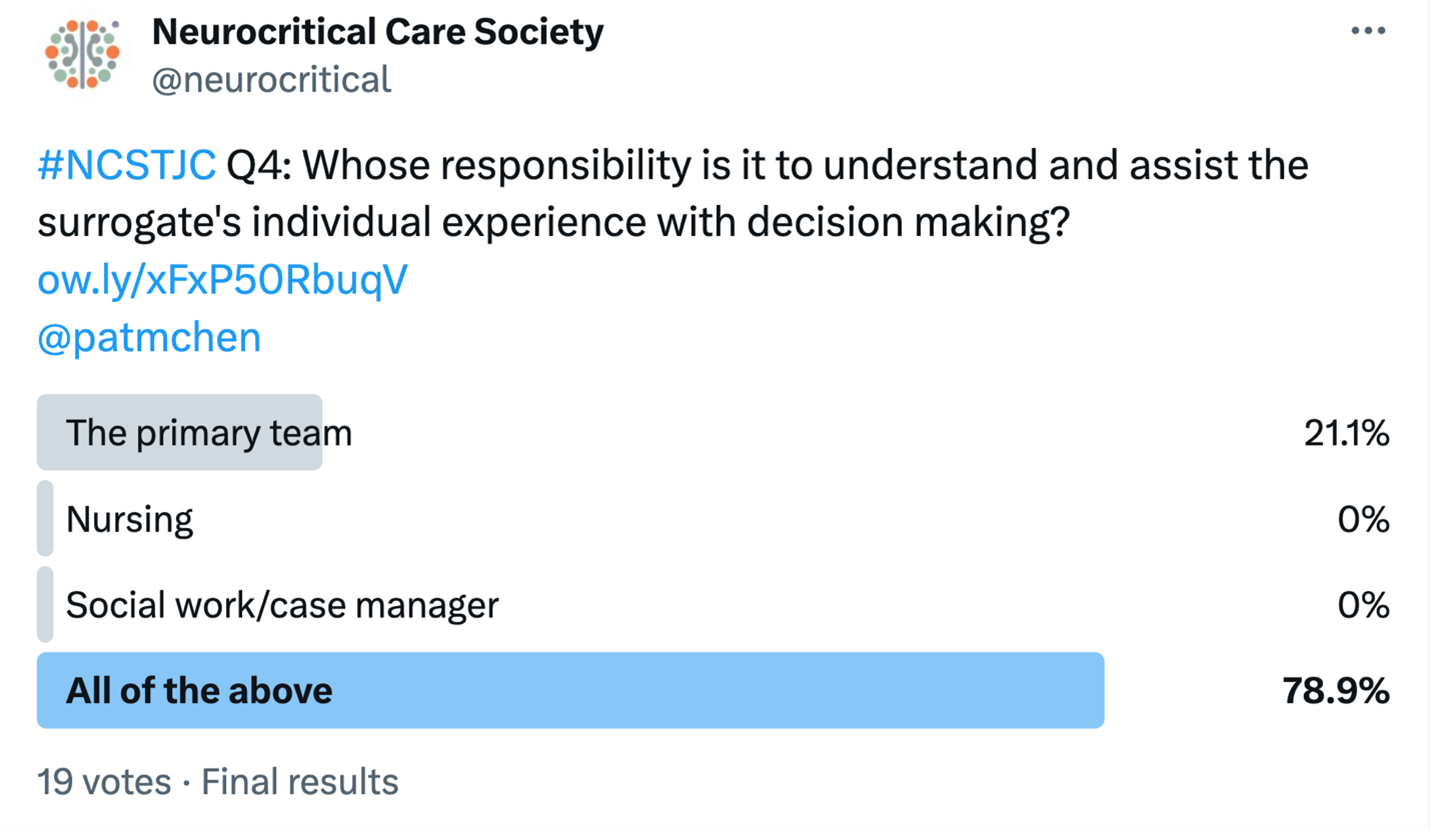
Question 4 was another poll, this time asking who bears the responsibility of understanding and assisting surrogates with their decision-making: 21.1% of respondents answered “the primary team,” while none said “nursing” or a “social worker/case manager” alone, and the remaining 78.9% answered “all of the above.” Everyone’s role as part of a multidisciplinary team in the ICU is clearly critical to the decision-making process, and participants recognized the need for all to be involved.
@NezerSara replied first: “burnout in caregivers is talked about a lot, but burnout while a family member is inpatient is not always as focused on; we have increased research in how we talk to patients and long-term effects and need more resources targeted at implementing & assessing this knowledge.” @rkchoi also replied, arguing that support groups have been beneficial in the stroke community and could also be beneficial for patients’ families in the ICU. Overall, it is clear that existing long-term support mechanisms may not be sufficient, and that there is a need for alternative options for families in the acute inpatient setting.
This concluded April’s NCSTJC, which featured a lively discussion emphasizing the importance of considering ethnicity in surrogate decision-making and illustrating the complexity of the subject. Additionally, it is crucial to ensure that surrogate decision-makers are well-equipped to represent patients’ wishes.
Read the article here: https://link.springer.com/article/10.1007/s12028-023-01724-2