NCS Twitter Journal Club Round-Up #NCSTJC: February 2024
Published on: May 24, 2024
The February edition of #NCSTJC features a fascinating article titled "Ceftriaxone to prevent early ventilator-associated pneumonia in patients with acute brain injury: a multicentre, randomised, double-blind, placebo-controlled, assessor-masked superiority trial." The article discusses the use of ceftriaxone as a preventative measure against hospital-acquired pneumonia in neurocritically ill patients.
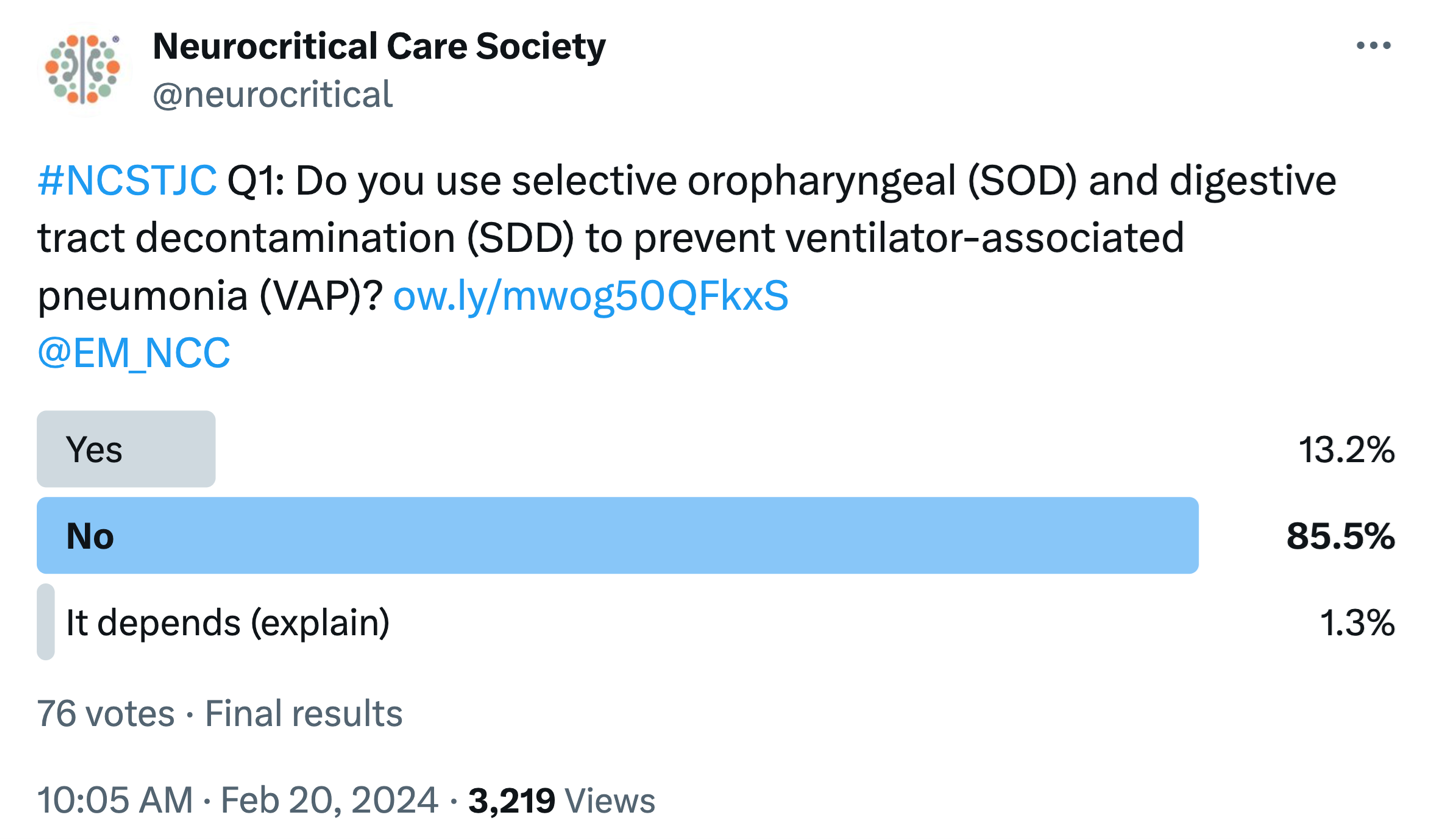
The discussion began by asking "Do you use selective oropharyngeal (SOD) and digestive tract decontamination (SDD) to prevent ventilator-associated pneumonia (VAP)?" The majority responded with "no" (85.5%), while 13.2% said "yes" and 1.3% answered "it depends". @EM_NCC quickly pointed out that the study sites in the article did not include these interventions. They instead used HOB elevation, monitored tracheal cuff pressure, performed oral care, changed filters/circuits only when necessary, initiated early enteral feeding, and administered stress ulcer prophylaxis. @KeatonSmetana answered by noting that his organization's ICU had chlorhexidine for VAP in their order set until recently. The current literature is now shifting towards just oral care. He also provided a link to a 2022 article outlining VAP prevention strategies.
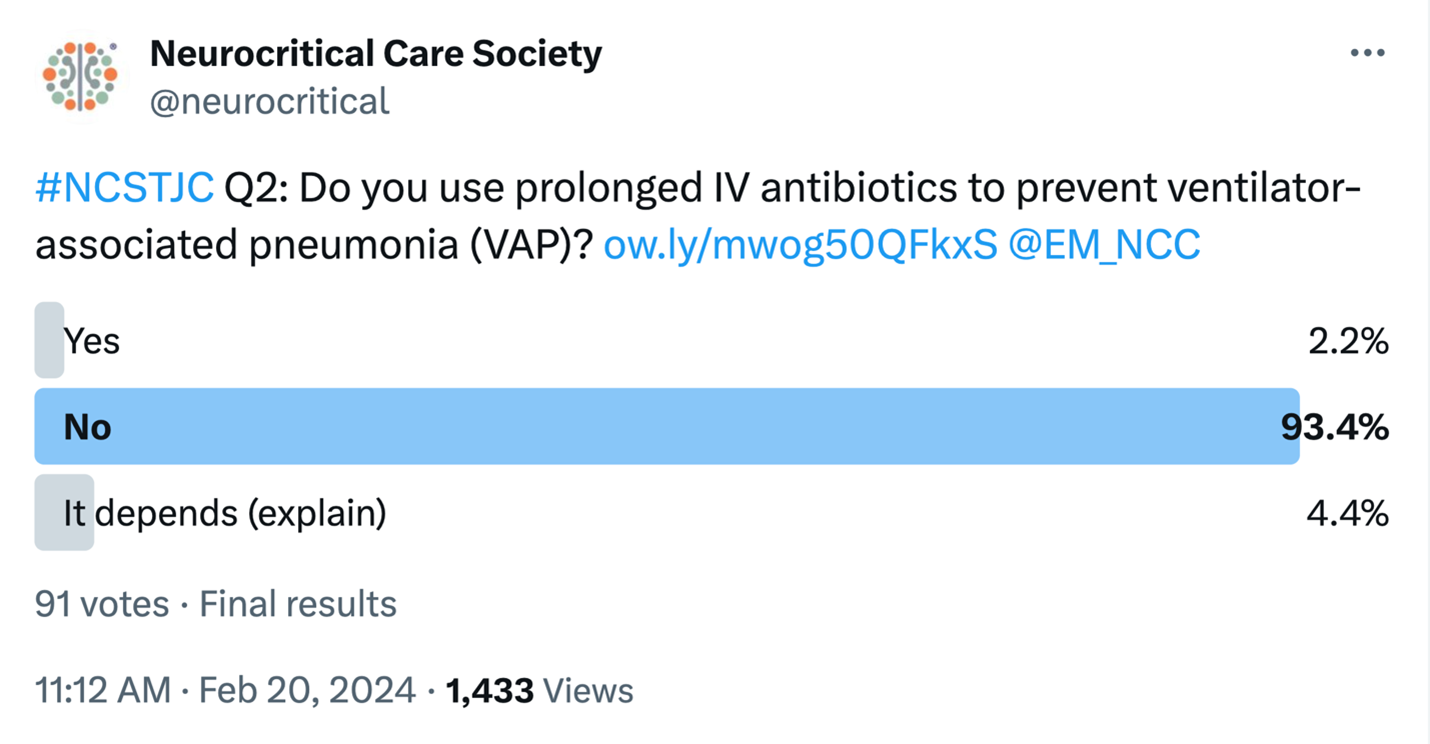
The subsequent poll then asked: “Do you use prolonged IV antibiotics to prevent ventilator associated pneumonia (VAP)?” Again, the majority of responders (93.4%) answered “No,” followed by “It depends” (4.4%) and “No” (2.2%). Given the overwhelming majority, little discussion was had on antibiotic selection or duration.
Question 3 asked participants, "What criteria do you use to diagnose ventilator-associated pneumonia (VAP)?" Respondents such as @SaadYazdaniMD, @gdomeni, and @EderCaceres5 were quick to refer to the ATS/IDSA recommendations. They also mentioned the importance of a thorough clinical examination and supplementary studies like X-rays and CT scans of the chest. @EM_NCC astutely asked, "Do you differentiate between ventilator-associated pneumonia and tracheobronchitis?"

Question 4 was a two-part query. It first asked: "Do you routinely screen for antibiotic-resistant organisms in your ICU patients?" This was followed by: "If so, which organisms and in what type of patients?" @Freemanwd was the first to respond by saying, "MRSA swab yes and 'CRE-RO' (Carbapenem Resistant Enterobacter, Rule Out) for patients coming from CRE+ locations." @EderCareres5 added that determining whether the patient has had a recent hospitalization or recent exposure to antibiotics is also part of the screening process. @EM_NCC referenced an article, saying, "4 of 9 PROPHY-VAP ICUs routinely screened for ESBL-producing bacteria on admission and discharge." @EricLawson90 shared that he does not routinely screen patients. However, he also expressed curiosity about whether local resistance patterns would affect the applicability of this study to local practice. @SaadYazdaniMD mentioned screening for MRSA and reiterated the IDSA guidelines. Finally, @gdomeni stated that they select antibiotics based on culture results.
The fifth question asked was: "Does the PROPHY-VAP trial's finding that a single dose of ceftriaxone decreased the incidence of early VAP in patients with acute brain injury affect your clinical practice?" @freemanwd started the discussion by saying "not yet" regarding changes in practice, adding that "the results seem almost too good to be true based on my number needed to treat calculations. We might hold an old school academic journal club among our city-wide neuroICU to dissect this article in detail later." @CamLeafloor commented, "for me, this paper changed my practice." @gdomeni echoed @freemanwd's sentiment about potentially changing his practice: "not really, because it needs to be proven in the real world."
The final question asked: "The authors also found that prophylactic ceftriaxone did not affect the incidence of late VAP in patients with acute brain injury. Does this finding change your clinical practice?" @EderCaceres5 responded: "Regarding VAP prevention, we don’t use prophylactic ceftriaxone in ABI. At least for now, I won't change my practice based on this study. However, it does open some perspectives and hypothesis in that sense." Both @salia_farrokh and @gdomeni agreed that the study was "hypothesis-generating," but it would not change their practice. @SaadYazdaniMD made a perceptive comment about the bacterial species and ceftriaxone coverage, stating that "some of the more prominent bugs causing early VAP identified in the study were E. coli, MSSA, and H. flu in the control group. Since the bugs for late VAP tend to be MDRs, I'm not sure that the lack of effect of prophylactic CTX on late VAP changes my perspective."
This month's article seems thought-provoking, although not necessarily practice-altering yet for many of the participants. Ventilator-associated pneumonia (VAP) can drastically affect patient outcomes in the ICU, underscoring the need for effective prevention methods. While the article presents promising information, it emphasizes the necessity for further research in this area.
Link to article: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(23)00471-X/abstract