NCS Journal Club Round-Up #NCSTJC: December 2023
Published on: March 29, 2024
 Moderator: @ZachThrelkeldMD
Moderator: @ZachThrelkeldMD
Link to Twitter Thread: https://twitter.com/neurocritical/status/1734592642845987281
NCS Twitter Journal Club for December 2023 featured a discussion about the article "Social Determinants of Health Attenuate the Relationship Between Race and Ethnicity and White Matter Hyperintensity Severity but not Microbleed Presence in Patients with Intracerebral Hemorrhage" by Bauman et al. It is a retrospective study that assessed the associations between social determinants of health and imaging biomarkers of microvascular disease. Previous studies noted the link between race and a higher prevalence of intracerebral vascular disease. The authors explored the relationship and suggested that socioeconomic factors, particularly education level, are additional risk factors for the disease, which may partially explain the racial disparity.
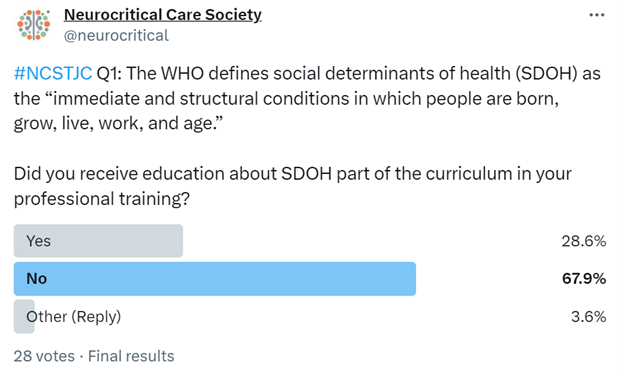
First, a definition of SDOH (social determinates of health) by the WHO as the “immediate and structural conditions in which people are born, grow, live, work, and age” set the stage. This was followed by a poll, asking, “did you receive education about SDOH as a part of the curriculum in your professional training?” @KeatonSmetana was the first to respond, stating his curriculum did not include formal teaching or discussion of SDOH. He was not alone. Of the 28 responders, 67.9% indicated a similar lack of a SDOH curriculum, 28.6% responded “yes,” and 3.6% responded “other.”
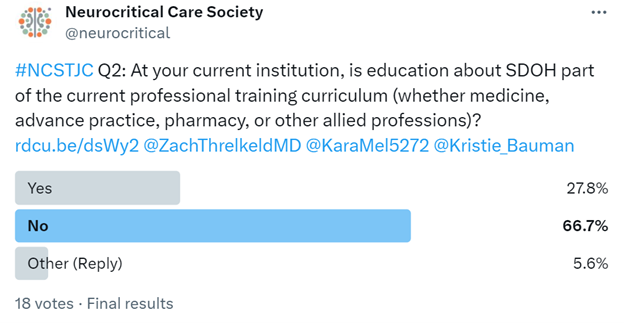
The second question was an additional poll that asked about Social Determinants of Health training at the hospital level. The question was, "At your current institution, is education about SDOH part of the current professional training curriculum (whether medicine, advance practice, pharmacy, or other allied professions)?" @EricLawson90 commented, "I haven't encountered a dedicated curriculum. I've mostly seen it taught as a component of a topic or in small scattered pieces. Developing a formal (longitudinal) curriculum can only enhance multidisciplinary #meded." The poll responses aligned with this comment, as 66.7% of participants also indicated that they did not have a dedicated curriculum. This left 27.8% of people with a dedicated curriculum and 5.6% who indicated other.
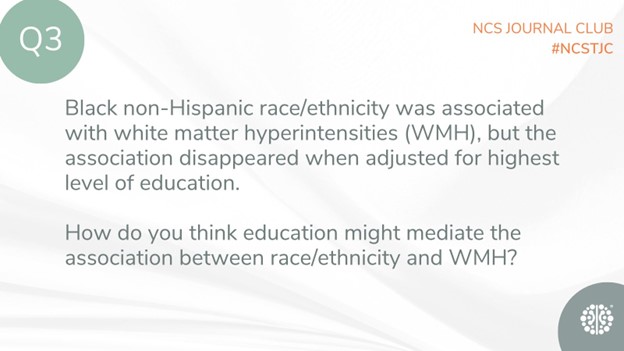
The subsequent question inquired about how the level of education may mediate the effect on white matter hyperintensities. @ZachThrelkeldMD noted the authors’ discussion in their article stating, “interesting finding -- the authors suggest that differences in highest level of education may reflect unequal distribution of resources more broadly. Similar disparities have been found in ischemic stroke and CV disease…”
Question 4 sparked discussion about the reason why factors such as current employment, income by zip code, and insurance status were not associated with microbleeds and white matter hyperintensities, but the level of education was. @EM_NCC remarked that the “Level of education may reflect aggregate exposure to risk factors / inequities contributing to WMH and cerebral microbleeds compared to a patient's current employment, insurance status, and median income by zip code.”
The final question urged readers to consider ways to improve their understanding of the social determinants of health that put patients at a higher risk for neurocritical illness. This is a challenging question, as highlighted by @KaraMel5272, who stated, "This is the question. And even more importantly, once we have achieved this understanding, how will we use it to create societal change to intervene and promote more equitable outcomes for patients with stroke and intracerebral hemorrhage (ICH).” The article, in its conclusion, reinforces a similar need for both awareness and understanding of SDOH to obtain more equitable outcomes for diverse patient populations.
The December edition of the #NCSTJC featured a fantastic discussion on the social determinants of health and their impact on risk factors for critical neurological illnesses, specifically white matter hyperintensities and microhemorrhages. The article emphasized the need for a comprehensive curriculum on these factors in both medical education and hospital settings. Understanding these factors is crucial for intervening and improving outcomes in the future.