Changing Names: The #NCSTJC is now the Neurocritical Care Society Virtual Journal Club (#NCSVJC)
Published on: June 24, 2025
A February 2025 Round-Up
To more accurately reflect the #NCSTJC expansion into other social media platforms, such as LinkedIn and Bluesky, we have updated the name to the Neurocritical Care Society Virtual Journal Club (#NCSVJC). Please join us monthly on X for the discussions with expansion to other social media platforms coming soon!

The February 2025 edition of the #NCSVJC was hosted by Dr. Richard Choi and again featured his unique #Tweetorial style of breaking down a journal article. The discussion was centered on the article “Efficacy and Safety and Andexanet Alfa Versus Four Factor Prothrombin Complex Concentrate for Emergent Reversal of Factor Xa Inhibitor Associated Intracranial Hemorrhage: A Systematic Review and Meta-Analysis,” which was published in October 2024 in the Neurocritical Care Journal.
Dr. Richard Choi kicked off the discussion with a review of Direct Oral Anticoagulants (DOAC), reminding participants they are now the preferred agent to reduce stroke risk in atrial fibrillation given their ease of use and decreased risk of bleeding. Their mechanism of action works either on thrombin or factor Xa.
When a major hemorrhage does occur in a patient taking a DOAC, Dr. Choi reminded us that it is important to undo the coagulopathy as soon as possible, linking to the 2022 AHA Guidelines on spontaneous ICH. Dabigatran has its own antidote, idarucizumab. The factor Xa inhibitors have many alternatives, including Andexanet alfa and 4-factor PCCs.
Dr. Choi reminded participants that the debate for which is better (Andexanet alfa vs 4-factor PCCs) is still a hotly debated topic and the authors of this month’s journal article attempted to answer the question by performing a meta-analysis which included a total of 16 studies. The authors found that anticoagulation reversal favored the use of Andexanet alfa, but that mortality data was limited by heterogeneity. They also noted more thromboembolic events in the Andexanet alfa group. Of the analyzed secondary outcomes, there were longer hospital stays in the Andexanet alfa group, and no difference in other outcomes between the two groups.
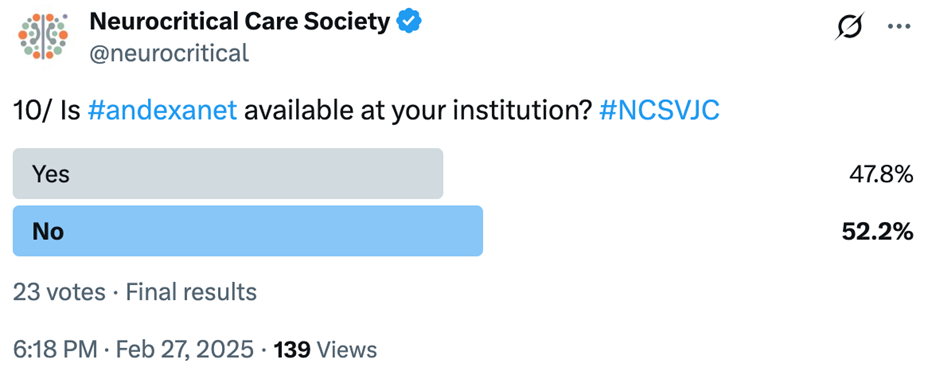
The first question directly to participants asked if Andexanet alfa is available at their institution. The responses were fairly split with equal numbers having it available versus not.
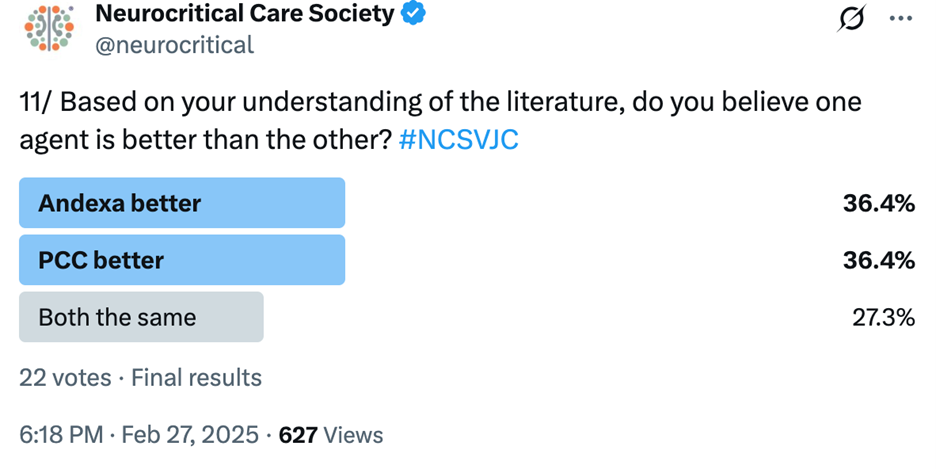
In the next poll, participants were asked which agent they understood to be better. The responses were equally divided between Andexanet alfa and PCC, which likely reflects the undetermined nature of the literature.
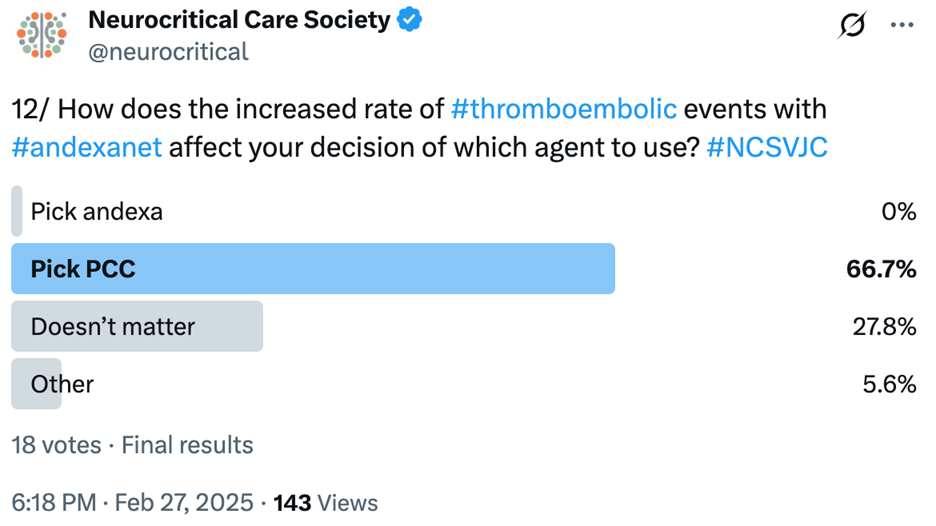
To better understand why participants are choosing a particular agent, the next poll asked if the increased rate of thromboembolic events with Andexanet alfa affected decisions on which agent to choose. Given these findings, no one said they would select Andexanet alfa, and a majority stated they would select PCCs.
To round out the discussion, the final question was: “Does the data from this paper change your preference of agent, and why?” @NG_Panos responded stating: “No this paper doesn’t change my mind. We need a RCT using a code ICH protocol (reverse within 60min) to compare both agents…” @rkchoi also directly weighed in stating: “I think we do need more data. I am curious to see what the FDA will end up deciding.”
The discussion on this meta-analysis by Sarhan et al. reflects the underlying sentiment for many clinicians that the literature is not decided on which agent for anticoagulant reversal is superior. This is further reflected by the varying use of Andexanet alfa across institutions.
Be sure to tune in to the next #NCSVJC!
Link to the full thread: https://x.com/neurocritical/status/1895135366396490056
Link to the article: https://link.springer.com/article/10.1007/s12028-024-02130-y