Why Racial Inequity Will Not End Until I Change
Published on: October 05, 2020
James Baldwin said, “Not everything that is faced can be changed, but nothing can change until it is faced.” Many who previously doubted the existence of racial inequity in our society now finally accept it as a grave problem. Sadly, many of the newly convinced fail to internalize the realization, thus perpetuating racial inequity by inaction.
Individual inaction often stems from the unconscious separation many create between “society” and our day-to-day lives. Compartmentalization of the racial inequity “out there” separate from our professional and personal lives perpetuates racial inequity. If we truly want change, each one of us must de-compartmentalize and act. What does de-compartmentalization and action mean for health care professionals? What does it mean for the Neurocritical Care Society (NCS)?
Action begins with gaining understanding of how racial inequity was created in the United States. The history of racial inequity begins with the arrival of the first enslaved Africans to Jamestown in 1619, continues through the de facto slavery imposed on African Americans between the Emancipation Proclamation of 1863 until the Civil Rights Act of 1968 on to the present day. As a result of economic and cultural segregation over many generations, Black Americans today have lower rates of homeownership, inherited wealth, opportunities for socioeconomic advancement and income, among other socioeconomic indices, relative to White Americans.
What about racial inequity, specifically regarding Black Americans, in the field of neurocritical care? Unlike racial representation data in many other areas of professional endeavor, statistics on Black Americans in this field are not readily available. However, available information suggests that racial inequity also exists among neurocritical care professionals. First, Blacks account for about half of the percentage of physicians and surgeons than they would if racial inequity did not exist, as shown in Figure 1. In contrast, gender disparities have almost disappeared.
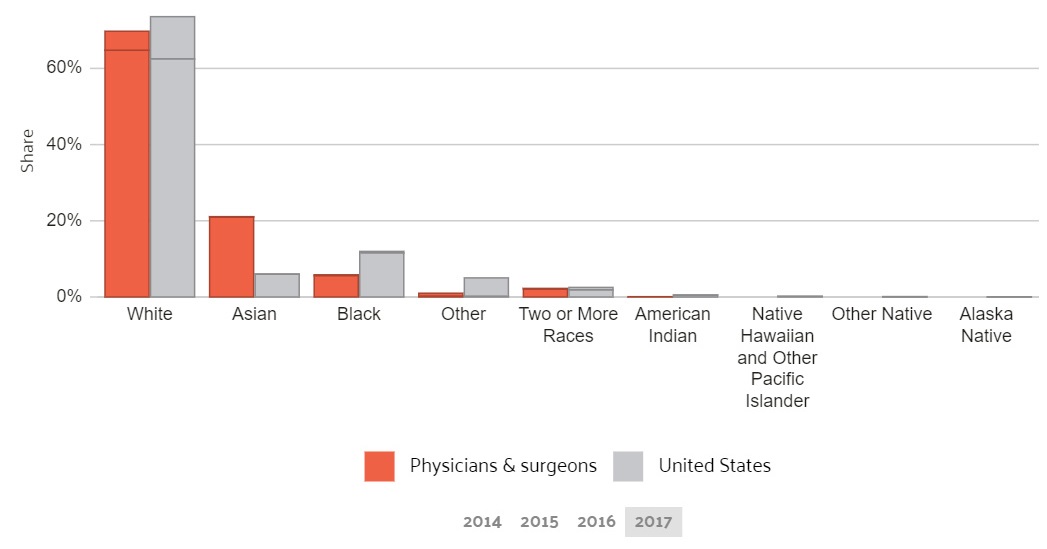
Figure 1. Data obtained by Data USA.
Lane-Fall, et al (Diversity in the Emerging Critical Care Workforce: Analysis of Demographic Trends in Critical Care Fellows from 2004–2014, published in Critical Care Medicine in 2017) stated the number of critical care fellows rose in that time period, but the percentage of Black critical care fellows remained unchanged (5% in 2004 compared to 4% in 2013-2014). Information on neurointensivists in practice or training is not readily available using public sources, such as PubMed. Navigating websites for the four groups endorsing the Neurocritical Care Boards (American Board of Anesthesiology, American Board of Emergency Medicine, American Board of Neurological Surgery, and the American Board of Psychiatry and Neurology) did not yield any data. Finally, the NCS website did not provide this information.
How can we address racial inequity among neurocritical care providers without rich and readily available information on racial representation in our profession? How can we change what we cannot see?
Diversity in the workforce matters. From the business to the entertainment world, inclusivity has yielded great gains in companies’ finances and corporate well-being and has improved product quality due to the broader set of perspectives on a given problem or idea that was achieved. Proven methodologies to increase diversity exist in business, entertainment arenas and in the sciences among others. As an example, the American Physics Society increased recruitment and retention of individuals from underrepresented racial, ethnic and socioeconomic groups using a methodical approach. For more information, see “Making Physics More Inclusive” by T. Hodapp and E. Brown (Nature 557, 629-632 (2018)).
In Neuroscience research, racial inequity is even deeper. As outlined in detail by Abiodun SJ in “Seeing Color, A Discussion of the Implications and Applications of Race in the Field of Neuroscience” published in August of 2019 in Front. Hum. Neuroscience, Blacks constitute a still exceedingly small percentage of researchers, tenured professors and funded researchers. Blacks remain underrepresented as research subjects. It is now recognized that many instances of past research in Black populations were unethical. Clearly, racial inequity exists not only in the clinical but in the research arenas of neurocritical care.
Increased racial diversity in neurocritical Care would help address some of the gaps in research into neurologic conditions such as stroke, depression and dementia, to name a few, that disproportionately impact Blacks. As an example of these health conditions, the American Heart Association in 2017 reported that the magnitude of association between systolic blood pressure (SBP) levels and stroke risk is three times greater in African Americans than in Whites; a 10–mm Hg difference in SBP is associated with an 8% (95% CI, 0–16) increase in the stroke risk in whites but a 24% (95% CI, 14–35) increase in non-Whites. Stroke mortality has fallen by 80% across all ages over the past 60 years, but no meaningful decrease in the magnitude of the African American to White racial disparity in stroke mortality has occurred in that time span.
A pooled analysis of ARIC and the CHS (Cardiovascular Health Study) showed that the RR of intracerebral hemorrhage for African Americans versus Whites was 5.8 at 45 years, 1.7 at 65 years, and 0.94 at 75 years of age.21 Among 45- to 64-year-olds in REGARDS, the incidence rate of intracerebral hemorrhage (per 100 000) was doubled for African Americans (46.0; 95% CI, 26.5–79.7) compared with Whites (21.5; 95% CI, 11.2–41.2).
Black Americans are less likely to receive anti-depressant therapy before completing suicide and less likely to receive second-generation antipsychotics than White Americans. Of relevance to police brutality, people with untreated mental illness are 16 times more likely to be killed in an encounter with law enforcement, as found by a report from the Treatment Advocacy Center in 2015. Addressing racial inequity in society would also indirectly improve stroke outcomes, as anticipated based on the fact that perceived racial discrimination is associated with all aspects of health, including hypertension, obesity, persistent inflammation and cardiovascular disease. Finally, healthcare delivery improves when patients and providers share similar perspectives and can communicate effectively, as shown in the SUCCEED study.
We can only change what we face. If we as neurocritical care professionals care about racial inequity, we must obtain and share a diagnostic overview of how racial inequity shows itself in our field. Once we face that, we can change.
NCS approved a diversity, equality and inclusion statement during its 2019 Board meeting, and this is integrated into the Strategic Plan for 2020-2022. In September 2020, the Board approved the new committee, Inclusion In Neurocritical Care (INCC), to oversee processes to increasing inclusiveness and advise the Society on methods to increase membership among the underrepresented. This committee receives reports from the Women In Neurocritical Care (WINCC), Sexual and Gender Minorities (SGM) and underrepresented Races and Ethnicities in Healthcare and Intersection Concepts (UREHIC) subcommitteees. This effort moves NCS closer to embracing its diversity and ensuring that all Society members are engaged in diversity efforts.