Using Transorbital Doppler and IMPRESSIT To Evaluate Intracranial Pressure in a Patient With Aneurysmal SAH
Published on: January 08, 2026
Clinical Case
A 66-year-old woman presented with sudden-onset headache and a brief loss of consciousness. CT head revealed diffuse aneurysmal subarachnoid hemorrhage (aSAH) with intraventricular hemorrhage. Vascular imaging confirmed a ruptured left anterior communicating artery aneurysm and several unruptured blister aneurysms. On arrival, she was lethargic but arousable and able to follow commands (Hunt and Hess grade III). A bedside external ventricular drain (EVD) was placed for cerebrospinal fluid diversion and intracranial pressure (ICP) monitoring, followed by craniotomy and aneurysm clipping the same day.
Over the next several days, the patient remained clinically stable. On hospital day 6, she acutely stopped following commands. CT angiography revealed mild vasospasm of the left internal carotid artery (ICA), and she underwent intra-arterial verapamil treatment via neurointerventional radiology with subsequent improvement. Of note, the patient lacked adequate transtemporal windows for transcranial doppler (TCD) vasospasm monitoring, so continuous video electroencephalography (cvEEG) was used to monitor alpha-delta ratios.
On hospital day 13, the EVD registered persistently elevated ICP values (22-44 mmHg). The patient did not exhibit new focal deficits or pupillary abnormalities. The discrepancy raised concern for EVD malfunction, possibly due to clot within the EVD catheter. The EVD, while draining in prior days, did have some fluctuation in the appearance of the waveform. To clarify whether the elevated readings were accurate, bedside TCD via the ophthalmic artery was performed to estimate ICP noninvasively using the IMPRESSIT method1,2.
POCUS Technique and Findings
Point-of-care ultrasound (POCUS) using TCD was performed using a high-frequency phase array probe with the patient in the supine position and eyes closed. Ultrasound gel was used over a transparent dressing placed over the eyelid to minimize pressure on the globe. Bilateral ophthalmic arteries (OA) and internal carotid arteries (ICA) were insonated through the closed eyelids in axial plane (Figure 1). Given the patient’s lack of transtemporal windows, MCA velocities could not be measured.
Peak systolic and end-diastolic velocities were measured for both OA and ICA. These values were applied to the IMPRESSIT equation which estimates cerebral perfusion pressure (CPPe) using the MCA diastolic and mean blood flow velocities (FVd and FVm respectively). The CPPe is then used to calculate ICP1,2,3:
CPPe = MAP*FVd /FVm + 14 = 58.8
ICP = MAP - CPP = 69-58 = 11
ICP was also calculated from the pulsatility index as a comparison4:
ICP = (10.93 x PI) - 1.28 = 12.8
These equations yielded an estimated ICP significantly lower than the EVD readings, supporting the hypothesis of inaccurate invasive measurements.
In light of this, neurosurgery elected to replace the EVD. The new catheter produced normal ICP values and improved waveform fidelity, confirming the prior device’s malfunction. There was a partially obstructing clot in the removed EVD catheter. CT scans were done in addition to TCD ICP calculation. Prior to the EVD being replaced, the CT showed slight worsening of hydrocephalus with an EVD tract hemorrhage and deep placement of the EVD. CT obtained after EVD replacement showed some improvement of the hydrocephalus. Immediately after EVD replacement, opening pressure was normal (8 mmHg) which was congruent with the calculated ICPs from TCD. It is likely that deep placement and clot found within EVD catheter caused falsely elevated ICP readings.
Discussion
This case illustrates how TCD can aid in resolving uncertainty in ICP measurements when EVD data and clinical findings diverge. Invasive ICP monitoring via EVD remains the gold standard, but its reliability depends on catheter patency and waveform fidelity. Obstruction by blood, debris, or biofilm can lead to false elevations, which may be difficult to recognize if the patient’s exam is limited or confounded. TCD is a noninvasive method of estimating ICP that has been validated in the neurocritical patient population. Certain circumstances such as lack of transtemporal windows preclude the ability to measure MCA velocities so in these clinic scenarios, transorbital Doppler may be more useful.
An important consideration when interpreting the formulas described by the IMPRESSIT-2 study is that they were developed primarily measuring the MCA, rather than the OA. The OA presents greater technical challenges for insonation. We did encounter difficulty insonating the intracranial ICA for comparison to the OA, despite using a phase-array probe which provides better depth than a linear probe. Although these formulas are well-established for using the MCA, our application required the inference that a similar relationship existed between the OA and the intracranial vessels. There are described proprietary formulas that measure the OA directly using the ratio of OA to ICA flow. Elevated ICP leads to orbital transmission of pressure, dampening OA flow and reducing the OA/ICA velocity ratio5,6. Another consideration for future application would be the inclusion of optic nerve sheath diameter (ONSD) measurement. Prior studies have shown that a combination of ONSD and TCD-estimated ICP provide a more accurate calculation7. In this case, measuring both optic sheaths multiple times would have been significantly more time-consuming than a bedside application of these formulas, but incorporation of ONSD information would potentially provide additional evidence to confirm presence of elevated ICP.
Technical considerations for this scan include:
- Use of a high-frequency probe with minimal pressure on the globe
- Patient should be supine with eyes closed and clear medical dressing over the eyelid
- For more specific measurements, adequate visualization of both OA and ICA flow profiles is necessary or MCA velocities.
- Doppler angles should be kept low (<60°) for accurate velocity assessment
Limitations of this method include operator dependency, variability in acoustic windows, and need for further validation across neurologic populations. Conditions such as orbital trauma, optic nerve pathology, or severe vasospasm may alter readings. Nonetheless, TCD can offer a physiologic, real-time complement to invasive monitoring.
In our case, the Doppler-based estimate aligned better with the patient’s clinical stability and imaging findings than the invasive EVD. These results directly influenced the decision to replace the EVD.
Conclusion
This case demonstrates the value of TCD with IMPRESSIT-derived ICP estimation in the assessment of suspected EVD malfunction, with an extrapolation of the equation on measurement of the OA rather than the MCA in the setting of poor transtemporal windows. In a patient with discordant ICP values, this POCUS technique provided actionable information that guided safe and effective care.
Figures
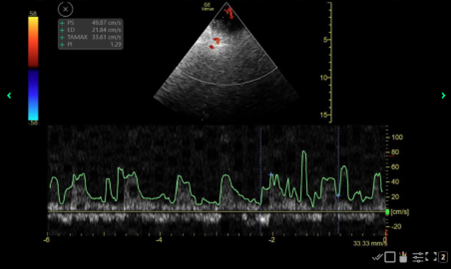
Figure 1: Shown here is a screenshot of the TCD waveform obtained from the left ophthalmic artery. The Mean Flow Velocity (MFV) (denoted by the TAMAX), End Diastolic Velocty (ED), and the Pulsatility Index (PI) from these measurements were used in the appropriate formulas along with a Mean Arterial Pressure (MAP) of 69 that was measured simultaneously to calculate the intracranial pressure (ICP). This is one screenshot, but several were taken (though not pictured) to ensure accuracy and appropriate capture of the measurements.
References
- Rasulo FA, Bertuetti R, Robba C, Lusenti F, Cantoni A, Bernini M, Girardini A, Calza S, Piva S, Fagoni N, Latronico N. The accuracy of transcranial Doppler in excluding intracranial hypertension following acute brain injury: a multicenter prospective pilot study. Crit Care. 2017 Feb 27;21(1):44. doi: 10.1186/s13054-017-1632-2. PMID: 28241847; PMCID: PMC5329967.
- Rasulo FA, Calza S, Robba C, Taccone FS, Biasucci DG, Badenes R, Piva S, Savo D, Citerio G, Dibu JR, Curto F, Merciadri M, Gritti P, Fassini P, Park S, Lamperti M, Bouzat P, Malacarne P, Chieregato A, Bertuetti R, Aspide R, Cantoni A, McCredie V, Guadrini L, Latronico N. Transcranial Doppler as a screening test to exclude intracranial hypertension in brain-injured patients: the IMPRESSIT-2 prospective multicenter international study. Crit Care. 2022 Apr 15;26(1):110. doi: 10.1186/s13054-022-03978-2. PMID: 35428353; PMCID: PMC9012252.
- Schmidt EA, Czosnyka M, Matta BF, Gooskens I, Piechnik S, Pickard JD. Non-invasive cerebral perfusion pressure (nCPP): evaluation of the monitoring methodology in head injured patients. Acta Neurochir Suppl. 2000;76:451-2. doi: 10.1007/978-3-7091-6346-7_93. PMID: 11450065.
- Bellner J, Romner B, Reinstrup P, Kristiansson K-A, Ryding E, Brandt L. Transcranial Doppler sonography pulsatility index (PI) reflects intracranial pressure (ICP). Surg Neurol. 2004;62(1):45-51. doi:10.1016/j.surneu.2003.12.007. PMID: 15226070
- Hamarat Y, Deimantavicius M, Kalvaitis E, Siaudvytyte L, Januleviciene I, Zakelis R, Bartusis L. Location of the internal carotid artery and ophthalmic artery segments for non-invasive intracranial pressure measurement by multi-depth TCD. Libyan J Med. 2017 Dec;12(1):1384290. doi: 10.1080/19932820.2017.1384290. PMID: 28982295; PMCID: PMC7182302.
- Lucinskas P, Deimantavicius M, Bartusis L, Zakelis R, Misiulis E, Dziugys A, Hamarat Y. Human ophthalmic artery as a sensor for non-invasive intracranial pressure monitoring: numerical modeling and in vivo pilot study. Sci Rep. 2021 Feb 26;11(1):4736. doi: 10.1038/s41598-021-83777-x. PMID: 33637806; PMCID: PMC7910574.
- Robba C, Pozzebon S, Moro B, Vincent J-L, Creteur J, Taccone FS. Multimodal non-invasive assessment of intracranial hypertension: an observational study. Crit Care. 2020;24(1):379. doi:10.1186/s13054-020-03105-z. PMID: 32591024. PMCID: PMC7318399