“Time Is Brain” for ICH Too!
Published on: May 13, 2024
Imagine you are a stroke clinician on call alone at night. Your pager goes off. Somehow, the jarring ringtone never fails to startle you. Code stroke. You sit bolt upright and quickly walk to the ER. You rush to get a NIHSS score between triage and the CT scanner. It’s at least a 21 for a left MCA syndrome. The patient’s last known well was only 45 minutes prior. A crowd encircles the CT technician as they scroll through the CT scan for the first time and it seems as if everyone is holding their breath.
An intracerebral hemorrhage (ICH) is seen in the left temporal lobe. Slowly, the emergency physician, the pharmacist, and the patient’s nurse file out of the room.
“Admit to neuro, right?” The emergency physician asks on their way out. As a stroke specialist, you are left to manage this patient alone and all sense of urgency seems to have disappeared.
If a large vessel occlusion had been seen and thrombolytics and embolectomy were on the table for an ischemic stroke, there would have been no collective exhale, and everyone involved would have been moving faster, not slower, to get this patient time-sensitive brain saving therapy.
Time is brain, right? Why does this sentiment not apply to ICH in the same way it does to the management of ischemic stroke? The answer is multifactorial and stems from a time in the not-so-distant past. The first trials supporting thrombolysis for ischemic stroke were published in the early 1990s and set off a cascade of time-based treatment metrics and standardization guidelines.¹ The ICH score was also developed around this time, and with its focus on an increasingly high mortality risk, may have inadvertently perpetuated a culture of pessimism, with some using this tool and others like it to justify limitations of aggressive care. (²,³,⁴) Meanwhile, studies on blood pressure control and surgical evacuation yielded inconclusive results that failed to definitively establish whether, and for whom, these treatments worked. (²,⁵)
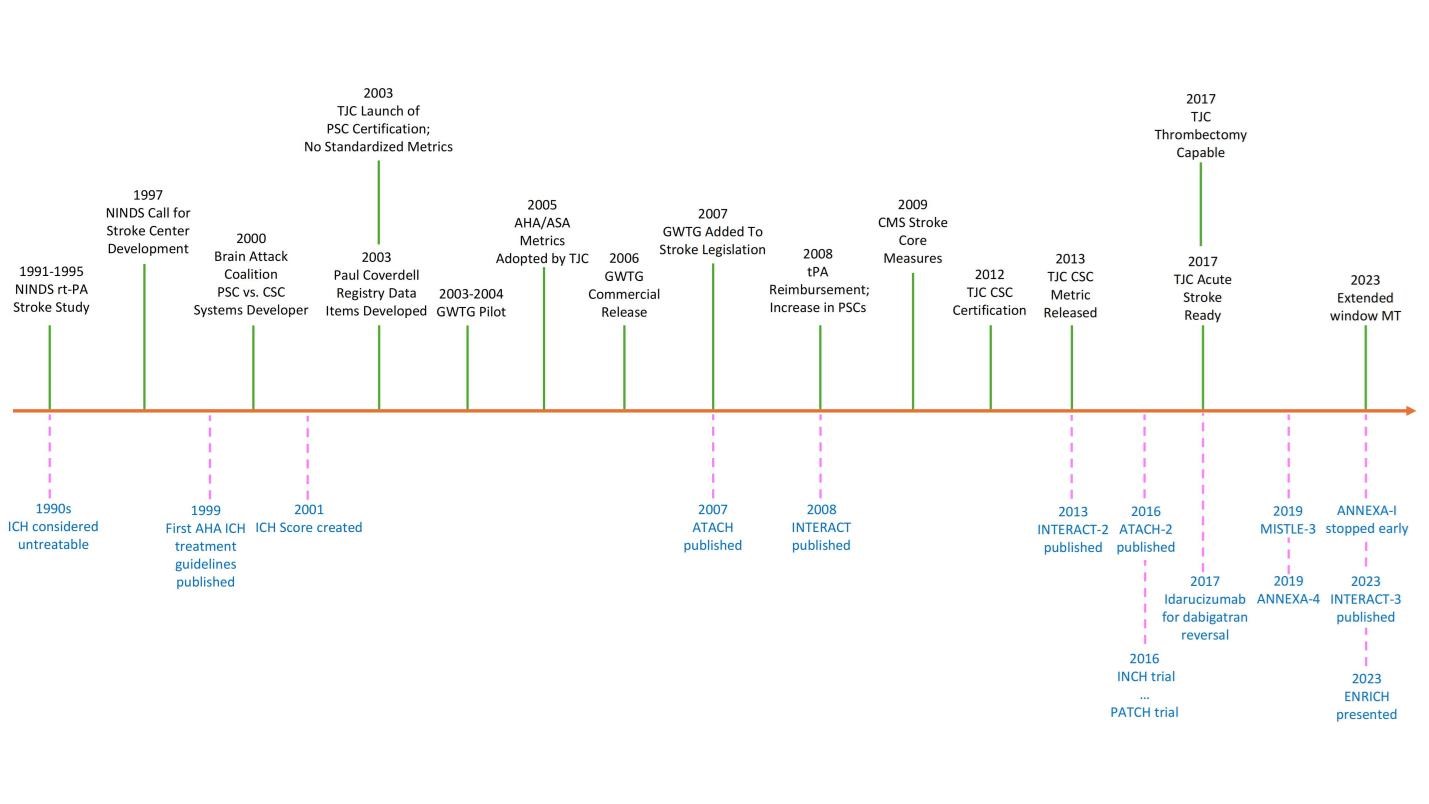
(Figure 1). As a result, it too often seemed as if there was no urgency in providing any particular treatment for patients with ICH.
Figure 1: A non-exhaustive timeline of milestones in the treatment of ischemic stroke vs. ICH since 1990, adapted from a graphic presented by Anne Alexandrov at the NCS Annual Meeting in 2022
Our recent paper published in Stroke, riding in the wake of recent trials supporting bundled ICH care and promising results from the ENRICH trial of minimally invasive hematoma evacuation, argues that time-based bundled care for ICH is the way of the future.⁵
Here are some key takeaways from this publication:
- There are a number of interventions now supported by recent evidence, with further evidence of their efficacy in combination as part of an ICH bundle of care.
- These treatments include:⁶
-
- Rapid and smooth blood pressure control without overcorrection
- Prompt and targeted anticoagulation reversal
- Consideration of minimally invasive surgical evacuation in some patients
- There is evidence that these interventions are more likely to be effective when they are initiated as soon as possible.
- Bundled care increases compliance with best practices, improves clinical outcomes, and should be adopted broadly across stroke centers.⁷
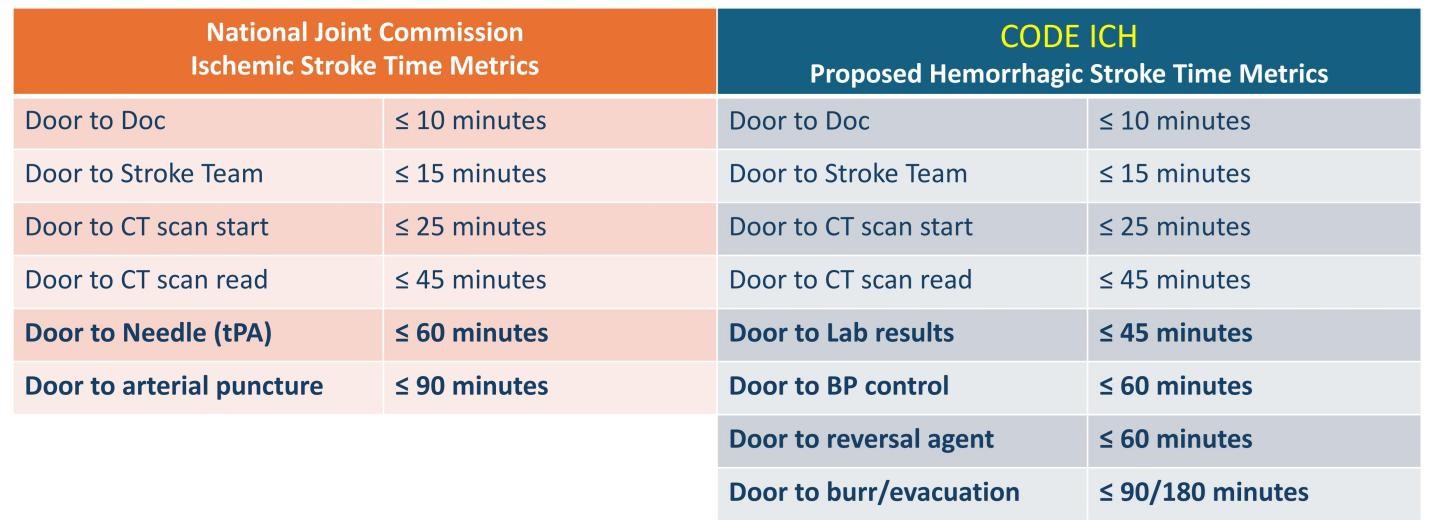
With this in mind, the acute management of ICH needs to catch up to that of ischemic stroke and should include blood pressure control, anticoagulation reversal, consideration of surgical intervention in some patients, and interdisciplinary and patient-centered application of bundled care (Figure 2). As always, further research is needed to better elucidate more specific treatment targets and facilitate more patient-tailored care. In the meantime, we advocate for accreditation bodies to adopt time-based metrics for the acute treatment of ICH akin to those of acute ischemic stroke (Figure 3).
For more information, please refer to Code ICH: A Call to Action, published in Stroke in December 2023.
Figure 2: Differences in Approaches.
Schematic comparison of how imaging, blood pressure control, hematologic therapy, and the role of surgical intervention currently differ between acute ischemic stroke (AIS) and intracerebral hemorrhage (ICH). BP indicates blood pressure; CTA, computed tomography angiography; EVT, endovascular therapy; and MIS, minimally invasive surgery. Originally published in Stroke, 2023.
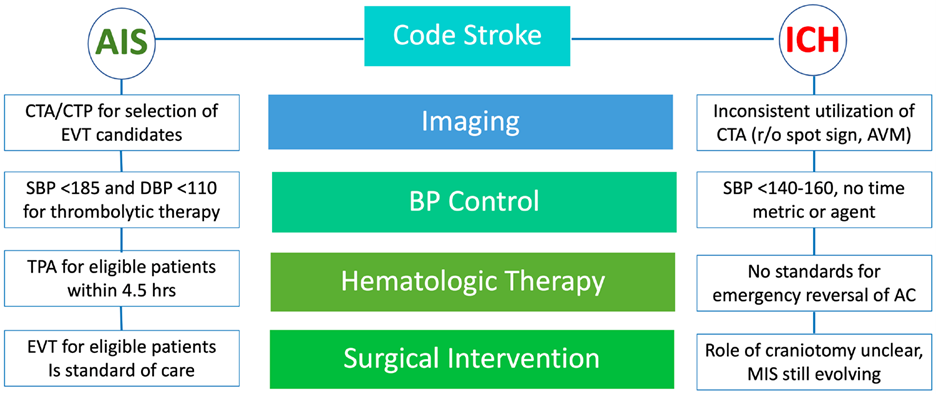
Figure 3: Proposed ICH Time Metrics. Originally presented at the NCS Annual Meeting in 2022 by Anne Alexandrov, Stephan Mayer, Joshua Goldstein, Jennifer Frontera, Christopher Kellner, and Sasha Yakhkind
References
1. Damani R. A brief history of acute stroke care. Aging (Albany NY). 2018 Aug 29;10(8):1797-1798. doi: 10.18632/aging.101542. PMID: 30157473; PMCID: PMC6128437.
2. Broderick JP, Grotta JC, Naidech AM, Steiner T, Sprigg N, Toyoda K, Dowlatshahi D, Demchuk AM, Selim M, Mocco J, Mayer S. The Story of Intracerebral Hemorrhage: From Recalcitrant to Treatable Disease. Stroke. 2021 May;52(5):1905-1914. doi: 10.1161/STROKEAHA.121.033484. Epub 2021 Apr 8. PMID: 33827245; PMCID: PMC8085038.
3. Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001; 32: 891–897.
4. Hemphill JC 3rd, White DB. Clinical nihilism in neuroemergencies. Emerg Med Clin North Am. 2009 Feb;27(1):27-37, vii-viii. doi: 10.1016/j.emc.2008.08.009. PMID: 19218017; PMCID: PMC2676162
5. Li Q, Yakhkind A, Alexandrov AW, Alexandrov AV, Anderson CS, Dowlatshahi D, Frontera JA, Hemphill JC, Ganti L, Kellner C, May C, Morotti A, Parry-Jones A, Sheth KN, Steiner T, Ziai W, Goldstein JN, Mayer SA. Code ICH: A Call to Action. Stroke. 2024 Feb;55(2):494-505. doi: 10.1161/STROKEAHA.123.043033. Epub 2023 Dec 15. PMID: 38099439.
6. Greenberg SM, Ziai WC, Cordonnier C; American Heart Association/American Stroke Association. 2022 Guideline for the Management of Patients With Spontaneous Intracerebral Hemorrhage: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2022 Jul;53(7):e282-e361. doi: 10.1161/STR.0000000000000407. Epub 2022 May 17. PMID: 35579034.
7. Ma L, Hu X, Song L, Chen X, Ouyang M; INTERACT3 Investigators. The third Intensive Care Bundle with Blood Pressure Reduction in Acute Cerebral Haemorrhage Trial (INTERACT3): an international, stepped wedge cluster randomised controlled trial. Lancet. 2023 Jul 1;402(10395):27-40. doi: 10.1016/S0140-6736(23)00806-1. Epub 2023 May 25. Erratum in: Lancet. 2023 Jul 15;402(10397):184. PMID: 37245517; PMCID: PMC10401723.