Role of Point-of-Care Ultrasound in Lumbar Puncture
Published on: January 22, 2024
INTRODUCTION
Despite major advances in neuroimaging, lumbar puncture (LP) remains a necessary diagnostic and therapeutic procedure for a variety of neurologic disorders. LPs aid in the diagnosis of central nervous system infection, subarachnoid hemorrhage, and many other disorders that can present as neurologic emergencies. As such, a delay in diagnosis caused by failed LP attempts may result in major morbidity or mortality.
Traditionally, LPs have been performed at the bedside without imaging guidance. However, many LPs are now being performed fluoroscopically in radiology departments due to an increasing shift toward more procedures performed by radiologists. In contrast, LPs performed by neurologists and neurosurgeons have significantly declined (by 74% and 83%, respectively).1 The most frequently described barriers to a successful bedside LP are age and body mass index (BMI). Age is associated with an increased risk of degenerative disease and spinal surgeries which lead to more challenging anatomy, while higher BMI has been associated with increased difficulty in identifying the proper intervertebral space.2-5 The ICU setting also poses its own challenges, as patients are critically ill, may be attached to a ventilator or other devices, and are often difficult to position.
Given the anatomical challenges associated with LPs, point-of-care ultrasound (POCUS) can serve as a helpful tool to improve success rates with bedside attempts.
CLINICAL CASE
A 77-year-old male was transferred to the intensive care unit from a rural hospital after he developed acute-onset confusion and abnormal behavior. He subsequently suffered a cardiac arrest in hospital with return of spontaneous circulation after resuscitation, then had a seizure. CT brain and basic work-up did not reveal a cause of his encephalopathy.
Cerebrospinal fluid sampling was sought as part of his evaluation. Positioning and landmark identification were challenging given the patient’s anatomy and intubated status. An LP was performed with ultrasound guidance to address these challenges. The static technique was used to identify landmarks for the procedure. A linear probe was used in the transverse orientation to locate a spinous process (Figure 1). Acoustic shadowing was identified, corresponding to the location of a spinous process (Figure 2). To demonstrate the differences between the two probes, a longitudinal view was subsequently obtained using a curvilinear probe (Figure 3). The spinous processes of L4 and L5 were identified, along with the sacrum (Figure 4).
A surgical marker was used on the patient’s skin to denote pertinent landmarks. These marks were then connected, with the point of intersection being identified as the optimal site for needle insertion. Basic cerebrospinal fluid parameters were within normal limits. Gram stain, culture and VZV/HSV PCR were negative as well. The patient was successfully extubated but suffered ongoing cognitive deficits. A subsequent MRI showed signs of hypoxic ischemic injury and an echocardiogram demonstrated signs of ischemic heart disease, which may have been the cause for his delirium and cardiac arrest.

Figure 1: Linear probe in transverse orientation with mark on patient’s skin to denote spinous process (red arrow).
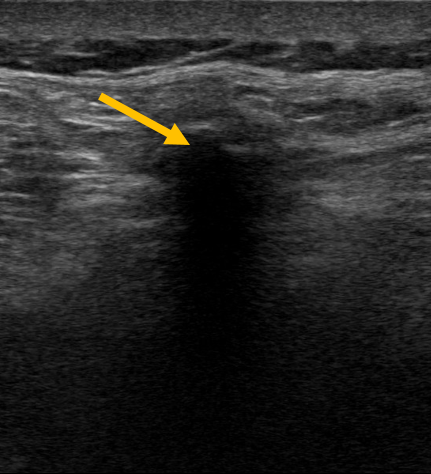
Figure 2: Linear probe demonstrating acoustic shadowing from a spinous process (yellow arrow).

Figure 3: Curvilinear probe in longitudinal orientation.
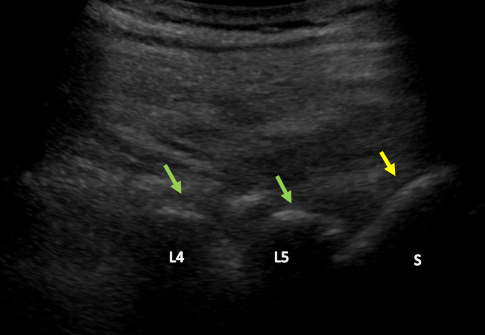
Figure 4: Longitudinal view with curvilinear probe demonstrating hyperechoic curved structures with acoustic shadowing, which are L4 and L5 (green arrows) and the sacrum (S) (yellow arrow).
DISCUSSION
In patients with difficult to palpate bony landmarks or unsuccessful initial attempts, POCUS-guided LP can be a useful tool to delineate patient anatomy and increase one’s chances of success at the bedside. A 2013 meta-analysis of 14 randomized controlled trials (RCTs) compared ultrasound-assisted LPs and epidural catheterizations with those performed using a traditional palpation landmark-based approach. This meta-analysis demonstrated a decreased risk of failed and traumatic LPs and epidural catheterizations when using ultrasound imaging.6 Although this study evaluated both LPs and epidurals, similar results were seen in a 2018 meta-analysis which only included RCTs involving LPs, and also demonstrated fewer traumatic LPs, decreased procedure duration, and lower patient pain scores.7 A more recent large retrospective cohort study in 2023 also showed that ultrasound-assisted LPs were associated with increased success rates and a lower risk of traumatic LP.8 Note, however, that the incidence of side effects after POCUS-guided LP such as post-LP headache, infection, or epidural bleeding have not yet been studied.
Ultrasound-guided LPs can be performed by a static or dynamic technique, with most comparative studies in the literature evaluating a static approach. 9-10 A dynamic, or real-time, ultrasound-guided LP is performed using a longitudinal (in-plane) or paramedian approach, and tracking the needle tip with insertion. A static-ultrasound-assisted LP (SULP) involves using the ultrasound to identify the bony landmarks to determine the ideal points of needle entry, and then proceeding with needle puncture without the ultrasound in hand. This can be performed with the patient in the sitting or lateral decubitus position.
The linear or curvilinear probe may be used for ultrasound-assisted LPs. The curvilinear probe may be preferred for patients with a higher BMI or larger body habitus for greater depth and increased field of view (Figure 3). The transverse view can be used to confirm and mark the midline (Figure 1). The longitudinal view, which can be obtained by rotating the probe 90 degrees, can be used to mark spinous processes and identify the interspinous/intervertebral spaces (Figures 3 & 4).
CONCLUSION
Lumbar punctures remain an important diagnostic and therapeutic tool for a variety of neurologic disorders. In patients with difficult to palpate bony landmarks or unsuccessful initial LP attempts, ultrasound can be a helpful tool to better delineate patient anatomy and improve one’s chances of success at the bedside.
References
- Kroll, H., Duszak, R., Nsiah, E., Hughes, D. R., Sumer, S., & Wintermark, M. (2015). Trends in lumbar puncture over 2 decades: A dramatic shift to radiology. American Journal of Roentgenology, 204(1), 15–19. https://doi.org/10.2214/ajr.14.12622
- Lin, N., Li, Y., Bebawy, J. F., Dong, J., & Hua, L. (2015). Abdominal circumference but not the degree of lumbar flexion affects the accuracy of lumbar interspace identification by Tuffier’s line palpation method: An observational study. BMC Anesthesiology, 15(1). https://doi.org/10.1186/1471-2253-15-9
- Halpenny, D., O’Sullivan, K., Burke, J. P., & Torreggiani, W. C. (2013). Does obesity preclude lumbar puncture with a standard spinal needle? the use of computed tomography to measure the skin to lumbar subarachnoid space distance in the General Hospital population. European Radiology, 23(11), 3191–3196. https://doi.org/10.1007/s00330-013-2909-8
- Jaime-Pérez, J. C., Sotomayor-Duque, G., Aguilar-Calderón, P., Salazar-Cavazos, L., & Gómez-Almaguer, D. (2019). Impact of obesity on lumbar puncture outcomes in adults with acute lymphoblastic leukemia and lymphoma: Experience at an academic reference center. International Journal of Hematology-Oncology and Stem Cell Research. https://doi.org/10.18502/ijhoscr.v13i3.1274
- Edwards, C., Leira, E. C., & Gonzalez-Alegre, P. (2015). Residency training: A failed lumbar puncture is more about obesity than lack of ability. Neurology, 84(10). https://doi.org/10.1212/wnl.0000000000001335
- Shaikh, F., Brzezinski, J., Alexander, S., Arzola, C., Carvalho, J. C., Beyene, J., & Sung, L. (2013). Ultrasound imaging for lumbar punctures and epidural catheterisations: Systematic review and meta-analysis. BMJ, 346(mar26 1). https://doi.org/10.1136/bmj.f1720
- Gottlieb, M., Holladay, D., & Peksa, G. D. (2018). Ultrasound‐assisted lumbar punctures: A systematic review and meta‐analysis. Academic Emergency Medicine. https://doi.org/10.1111/acem.13558
- Short, A., Dunneback, E., Stephens, J. R., Guidici, J., Chatterjee, A., Finn, E., Contarino, M., Spangler, H., Heath, J., McEntee, J., Donohoe, A., Hemsey, D., Moore, C., Sturkie, E., Kumfer, A. M., Campbell, R. A., & Dancel, R. (2023). Safety and predictors of the success of lumbar punctures performed by a Medicine Procedure Service. Journal of Hospital Medicine. https://doi.org/10.1002/jhm.13143
- Li, Y., Carandang, R. A., Ade, S., Flahive, J., & Daniello, K. (2019). Ultrasound-guided lumbar puncture improves success rate and efficiency in overweight patients. Neurology: Clinical Practice, 10(4), 307–313. https://doi.org/10.1212/cpj.0000000000000725
- Soni, N. J., Franco-Sadud, R., Schnobrich, D., Dancel, R., Tierney, D. M., Salame, G., Restrepo, M. I., & McHardy, P. (2016). Ultrasound guidance for lumbar puncture. Neurology: Clinical Practice, 6(4), 358–368. https://doi.org/10.1212/cpj.0000000000000265
Author Affiliations
- Izn Shahab, MD, Gary Hunter, MD, Erika Sigman, MD: University of Saskatchewan, Saskatchewan, Canada
- Earllondra Brooks, MD: Emory University School of Medicine, Atlanta, Georgia