Point of Care Ultrasonography: An Indispensable Tool for the Neurocritical Care Team
Published on: December 27, 2017
Vascular access with point of care ultrasonography (POCUS) is now considered to be standard of care and has greatly reduced iatrogenic complications of central venous access.1 Although POCUS is an essential skill for all critical care providers, it extends beyond the use of ultrasound guidance for vascular access. POCUS in critical care can facilitate timely cardiovascular and hemodynamic assessments of critically ill patients. Diagnostic applications of POCUS in critical care include assessment of lung, cardiac and vascular ultrasound for clinical conditions such as pneumothorax, pulmonary edema, pleural effusion, consolidation syndrome (pneumonia and atelectasis), left and right systolic ventricular dysfunction, pericardial tamponade, intravascular volume assessment and fluid responsiveness, pulmonary embolism, and cardiac arrest. Bedside critical care ultrasound assessment can provide critical information to guide time sensitive decision making about acute cardiopulmonary emergencies while awaiting laboratory tests or definitive imaging in critically ill patients.2 Major advantages of POCUS include lack of radiation, portability with ease of use, ability to record images, good reproducibility, cost efficiency and ability to serially evaluate cardiopulmonary status.
Real-time interpretation and easily available ultrasound machines are now considered vital to our “contemporary critical care practice.” Guidelines regarding education, credentialing and competence have been released by several organizations including the Society of Critical Care Medicine (SCCM) and The World Interactive Network Focused on Critical UltraSound (WINFOCUS). Expected basic skill set for POCUS include recognizing the presence of pericardial effusion, severe right and left ventricular dysfunction, regional wall motion abnormalities (to correlate with territories perfused by each coronary artery and potential associated myocardial ischemia), gross anatomical valvular abnormalities, and assess the size and collapsibility of the inferior vena cava (IVC) to identify preload responsiveness (acknowledging certain limitations like: RV dysfunction or Vt> 8ml/kg). An expert-level physician is expected to be competent in both transthoracic and transesophageal echocardiography and be able to use advanced modes like color doppler, spectral mode, tissue doppler, and to use contrast and/or bubbles to assess pulmonary hypertension, diastology, and mechanical valvular dysfunction.3,4 Furthermore, the upcoming National Board certification in critical care echocardiography is planned with an initial examination to be administered in January 2019 and followed by a certification process yet to be determined.5
Knowledge and competency in POCUS has specific advantageous applications in neurocritical care. Patients with stroke, trauma or subarachnoid hemorrhage (SAH) are predisposed to multiple cardiopulmonary complications such as evolving neurogenic stunned myocardium or stress cardiomyopathy with subsequent congestive heart failure and hydrostatic pulmonary edema; neurogenic pulmonary edema: or aspiration pneumonia. Many of such patients require frequent assessments and interventions for fluid status as part of their critical care management. Hence, they are predisposed to shock from multiple etiologies (i.e., sepsis, cardiac, vasoplegia or neurogenic). POCUS echocardiography performed by intensivists can be potentially life-saving in patients with new onset acute respiratory failure or shock in patients with acute brain injury. Echocardiography is recommended as the first modality of choice in diagnosis and management of undifferentiated shock.6 The core types of shock can be easily distinguished using POCUS multiple protocols such as Rapid Ultrasound in Shock and Hypotension (RUSH), Focused Assessment with Transthoracic Echocardiography (FATE)7 or Focused Ultrasonography in Surgical Anesthesia (FUSA) in the perioperative period.8 Further, POCUS can also provide important ongoing hemodynamic monitoring during resuscitation by assessing fluid responsiveness and pulmonary edema in response to therapy. In patients with acute dyspnea or hypoxia, POCUS using Bedside Lung Ultrasound in Emergency (BLUE) protocol can help with rapid diagnosis of pulmonary edema, pneumothorax, pneumonia, atelectasis and initiate targeted treatment.9 The Focused Echocardiography Evaluation in Life Support (FEEL) during cardiac arrest can help institute targeted treatment rapidly in addition to ACLS support.10
In addition, POCUS might help in identifying emergent underlying etiology in patients presenting with acute ischemic stroke, like LV thrombus, aortic dissection or decompensated heart failure. In patients with SAH, cardiac POCUS can help to tailor volume resuscitation, diagnose and monitor patients with acute hypotension or pulmonary edema caused by stress cardiomyopathy as inotrope and vasopressors titration is feasible with serial echocardiography assessments. In patients at risk of developing worsening cerebral edema and impending cerebral herniation, POCUS of optic nerve sheath can be used to identify patients with worsening intracranial hypertension.11 Transcranial doppler (TCD) POCUS assessments can be used to serially monitor evolving vasospasm in subarachnoid hemorrhage patients or evolving cerebral perfusion patterns as surrogates for malignant cerebral edema in patients at risk of cerebral circulatory arrest.12 This can be used to guideosmotic therapy in primary acute brain injury or provide ancillary information in post cardiac arrest patients.
Illustrative Case
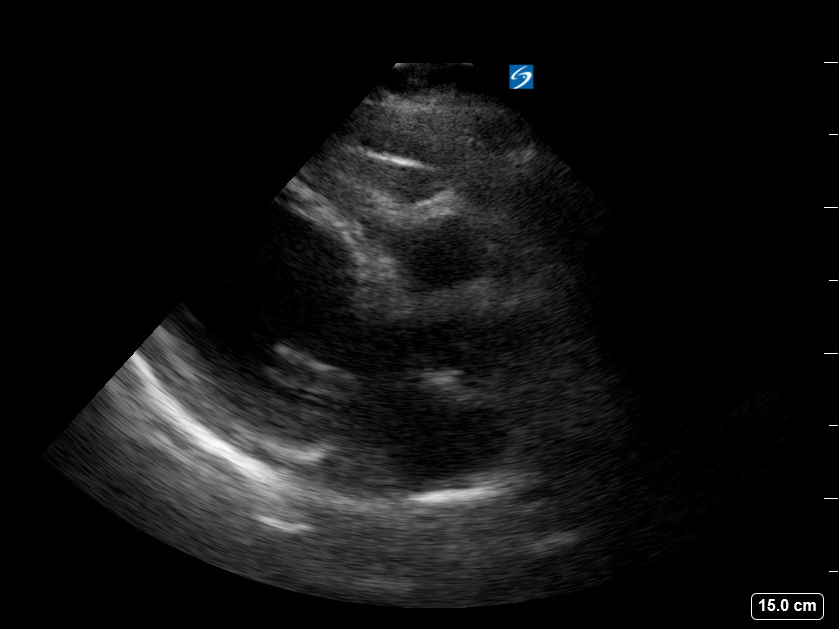
A 56-year-old female with no prior medical history presented with Hunt Hess 3, Modified Fisher 4 SAH due to a ruptured anterior communicating aneurysm. POCUS echocardiography on admission showed unremarkable heart with good ejection fraction. Aneurysm was protected by coiling. On post bleed day four, she was found to have elevated TCD velocities suspicious for vasospasm in the setting of new speech difficulties. Pressure augmentation was initiated using vasopressors. A subclavian central venous catheter was inserted and followed by increasing dyspnea, acute hypoxic respiratory failure and persistent arterial hypotension. Lung ultrasound showed normal pleural sliding in all lung regions, so pneumothorax was ruling out. However, multiple B lines (See Figure 1) were apparent and suggestive of pulmonary edema. POCUS echocardiographyrevealed a dilated left ventricle with poor contractility and apical ballooning consistent with Takutsubo cardiomyopathy (See Figure 2) and plethoric IVC without significant respiratory variability. Based on these findings, a diagnosis of decompensated systolic heart failure caused by stress cardiomyopathy. Intravenous fluids were discontinued, and inotropic support was started with successful blood pressure augmentation. The patient’s respiratory status improved, and she was taken for angioplasty. All this was completed by bedside within one to two hours’ time frame from initial new neurological symptoms appearance. This entire evaluation was performed by a competent neurocritical care team in POCUS. Over the next few days, volume and blood pressure augmentation was titrated using serial cardiac and lung POCUS assessments. By the second week of medical management, the patient’s TCDs normalized, systolic function improved and the patient was discharged to floor for further clinical follow up.
Resources to Learn POCUS
Neurocritical Care Society (NCS) offers a POCUS workshop at the annual national meeting to teach clinical applications of ultrasound. There are many POCUS related high quality free open access medical education resources available on the internet and on social media (Twitter #ultrasound #POCUS #FOAMed).
We encourage the members of NCS to submit interesting cases where POCUS has helped in management of their patients for publication in subsequent issues of Currents. Please contact NCS if you are interested in participating in the ultrasound workshop at the 2018 annual meeting.
Figure 1: Lung ultrasound showing B-lines consistent with pulmonary edema
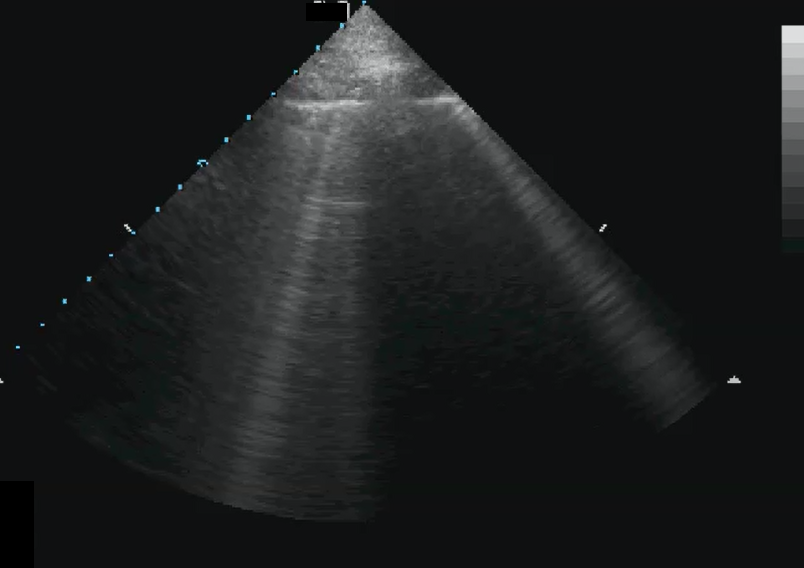
Figure 2: POCUS echocardiography showing parasternal long axis view with dilated apex and poor contractility
Bibliography
- Saugel, B., Scheeren, T. W. L. & Teboul, J.-L. Ultrasound-guided central venous catheter placement: a structured review and recommendations for clinical practice. Crit. Care 21, (2017).
- Ha, Y.-R. & Toh, H.-C. Clinically integrated multi-organ point-of-care ultrasound for undifferentiated respiratory difficulty, chest pain, or shock: a critical analytic review. J. Intensive Care 4, (2016).
- Frankel, H. L. et al. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients—Part I: General Ultrasonography. Crit. Care Med. 43, 2479–2502 (2015).
- Levitov, A. et al. Guidelines for the Appropriate Use of Bedside General and Cardiac Ultrasonography in the Evaluation of Critically Ill Patients—Part II: Cardiac Ultrasonography. Crit. Care Med. 44, 1206–1227 (2016).
- Díaz-Gómez, J. L., Frankel, H. L. & Hernandez, A. National Certification in Critical Care Echocardiography: Its Time Has Come. Crit. Care Med. 45, 1801–1804 (2017).
- Cecconi, M. et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 40, 1795–1815 (2014).
- Jensen, M. B., Sloth, E., Larsen, K. M. & Schmidt, M. B. Transthoracic echocardiography for cardiopulmonary monitoring in intensive care. Eur. J. Anaesthesiol. 21, 700–707 (2004).
- Focused cardiac and lung ultrasonography: implications and applicability in the perioperative period. Romanian J. Anaesth. Intensive Care 23, (2016).
- Lichtenstein, D., Van Hooland, S., Elbers, P. & Malbrain, M. L. N. G. Ten good reasons to practice ultrasound in critical care. Anestezjol. Intensywna Ter. 46, 323–335 (2014).
- McLean, A. S. Echocardiography in shock management. Crit. Care 20, (2016).
- Rajajee, V., Vanaman, M., Fletcher, J. J. & Jacobs, T. L. Optic Nerve Ultrasound for the Detection of Raised Intracranial Pressure. Neurocrit. Care 15, 506–515 (2011).
- Kalanuria, A., Nyquist, P. A., Armonda, R. A. & Razumovsky, A. Use of Transcranial Doppler (TCD) Ultrasound in the Neurocritical Care Unit. Neurosurg. Clin. N. Am. 24, 441–456 (2013).