Making a Case for Ketamine in Pediatric Status Epilepticus
Published on: January 16, 2025
Status epilepticus (SE) is one of the most common neurological emergencies in children, with 23 cases per 100,000 children and a mortality of up to 7%1. Children are at a particularly elevated risk for refractory status epilepticus (RSE), with up to 40% of pediatric cases developing RSE.2 Furthermore these cases have a greater mortality, with a rate as high as 44%.3 It is therefore imperative to appropriately diagnose and treat these patients in a timely manner. The selection of medications to treat SE in children is of the utmost importance, as particular pediatric populations are especially vulnerable to the adverse effects of certain antiseizure medications (ASMs) (e.g. valproic acid) and anesthetic infusions (e.g. propofol).
The use of ketamine for SE has gained renewed interest in the realm of pediatric neurocritical care in recent years. These efforts culminated in a meta-analysis we published earlier this year, featuring the possible role of ketamine in the management of SE in children.4 The following patient case highlights the advantages of ketamine as a potentially safer alternative to traditional GABAergic anesthetic infusions (e.g., benzodiazepines, propofol, and barbiturates) in a patient population particularly vulnerable to their deleterious adverse effects.
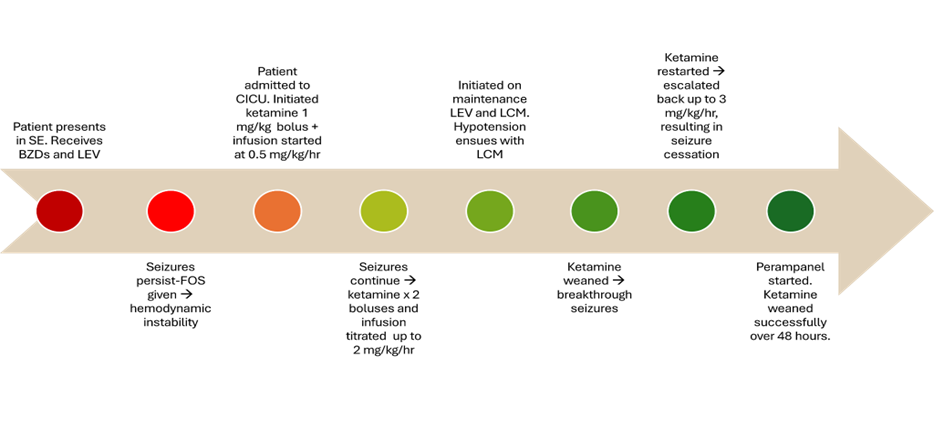
A 2-year-old male with a history of hypoplastic left heart syndrome status post Norwood procedure presents to the hospital with right-sided focal seizures. Despite receiving multiple doses of benzodiazepines (BZDs) and a loading dose of levetiracetam (LEV) in the ED, his seizures persist. In an attempt to control his seizures, he then receives a loading dose of fosphenytoin (FOS) which leads to severe hypotension and hemodynamic instability. An epinephrine infusion is initiated, and the patient is admitted to the cardiac ICU (CICU), where he continues to have episodes of right arm shaking and eye deviation every 2-3 minutes.
A multidisciplinary discussion ensues between the neurocritical care team and the cardiac critical care team about the risks and benefits of escalation of therapy with anesthetic infusions. Of note, the moment of intubation (and initiation of positive pressure ventilation) poses a particular risk because of the patient’s unique physiology. Therefore, the decision is made to trial ketamine without intubation. He receives a 1 mg/kg bolus of ketamine and is started on a ketamine infusion at 0.5 mg/kg/hr. Two additional 1 mg/kg boluses are administered due to persistent seizures, and his infusion is uptitrated by 0.5 mg/kg/hr increments until achieving a rate of 2 mg/kg/hr. At that point his clinical seizures subside, and his EEG is negative for subclinical seizures. His vital signs stabilize and remain normal, except for some intermittent mild hypertension and tachycardia. During this time, he remains on 4 L of 25% FiO2. He is initiated on maintenance LEV and lacosamide (LCM). Upon administration, the LCM results in profound hypotension and is subsequently discontinued. Ketamine is weaned 48 hours later, but due to breakthrough seizures is again restarted and escalated to 3 mg/kg/hr with resultant seizure cessation. After consultation with the epilepsy service, the decision is made to start perampanel (PER) via gastrostomy tube. After 48 hours of PER therapy, ketamine is weaned again over the course of 48 hours without further seizure recurrence. A few days later, the patient is discharged home with fewer than two short seizures a day, on a maintenance ASM regimen of PER and LEV, and a planned follow-up outpatient visit with pediatric neurology.
This patient case highlights the clinical implementation of ketamine based on our recent meta-analysis supporting the use of ketamine for pediatric SE.4 In this study published in Epilepsia, we demonstrated that the addition of ketamine resulted in cessation of SE in 51% of cases. While this is similar to the clinical effectiveness of other infusions, there is an additional safety benefit, as none of the included studies reported significant side effects with the use of ketamine. Only minor and/or rare side effects were reported, including increased oral secretions, hypertension, and delirium.
When evaluating the specific patient factors from the case above in the context of our meta-analysis, a few noteworthy details should be highlighted. First, in terms of seizure types, most patients had focal seizures with secondary generalization in three of the included studies5,6,7, which was the case for the patient presented here. Second, some patients receiving ketamine never required intubation. In the largest cohort included in the meta-analysis, Jacobwitz and colleagues found that 4% of patients who received ketamine were not intubated8. Although this is not a large number, it is more notable to recognize that most patients were already intubated before ketamine initiation, and that other anesthetic infusions ubiquitously require intubation. Meanwhile, a study by Ilvento et al. found that the majority of patients from their cohort did not require intubation9. In the case above, one of the biggest benefits of ketamine for this patient was circumventing the need for a potentially risky intubation. In addition, given his cardiovascular history and episodes of profound hemodynamic instability with other ASMs that required vasopressors and admission to the CICU, there was concern that other anesthetic infusions could exacerbate his cardiovascular pathophysiology. Of note, in the aforementioned study by Jacobwitz et al., only 35% of patients receiving ketamine developed hypotension, of whom 92% developed hypotension prior to ketamine initiation (with their hemodynamics eventually stabilizing after the initiation of ketamine)8. These considerations factored into the decision to trial ketamine in the case presented above. While ketamine proved effective in this case, the potential risks and benefits of ketamine for patients with SE and concurrent underlying cardiovascular disease should be evaluated on a case-by-case basis.
Although our meta-analysis distilled the available literature for ketamine in pediatric SE, it is important to recognize that the quality of evidence of the studies included remains low, with no clinical trials currently available. The only clinical trial attempted thus far was halted due to poor recruitment8. Nevertheless, ketamine remains a promising option for pediatric patients, but more research is necessary to better elucidate its role in the treatment of pediatric SE and RSE, ideally with randomized controlled trials.
References
- Barzegar M, Mahdavi M, Galegolab Behbehani A, Tabrizi A. Refractory Convulsive Status Epilepticus in Children: Etiology, Associated Risk Factors and Outcome. Iranian journal of child neurology [Internet]. Shahid Beheshti University of Medical Sciences; 2015 Oct 8;9(4):24–31. Available from: https://journals.sbmu.ac.ir/ijcn/article/download/7173/7809
- Chin RFM, Neville BGR, Peckham C, Bedford H, Wade A, Scott RC. Incidence, cause, and short-term outcome of convulsive status epilepticus in childhood: prospective population-based study. The Lancet [Internet]. Elsevier; 2006 Jul 15;368(9531):222–229. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(06)69043-0/fulltext
- Sahin, M., Menache, C. C., Holmes, G. L., & Riviello Jr, J. J. (2001). Outcome of severe refractory status epilepticus in children. Epilepsia, 42(11), 1461-1467.
- Chiriboga N, Spentzas T, Abu‐Sawwa R. A systematic review and meta‐analysis of ketamine in pediatric status epilepticus. Epilepsia. Wiley-Blackwell; 2024 Jun 17;
- Gaspard N, Foreman B, Judd LLM, Brenton JN, Nathan BR, McCoy B, Al-Otaibi A, Kilbride R, Fernández IS, Mendoza L, Samuel S, Zakaria A, Kalamangalam GP, Legros B, Szaflarski JP, Loddenkemper T, Hahn CD, Goodkin HP, Claassen J, Hirsch LJ, LaRoche SM. Intravenous ketamine for the treatment of refractory status epilepticus: A retrospective multicenter study. Epilepsia [Internet]. NIH Public Access; 2013 Aug 1;54(8):1498–1503. Available from: https://pubmed.ncbi.nlm.nih.gov/23758557/
- Rosati A, L’Erario M, Ilvento L, Cecchi C, Pisano T, Mirabile L, Guerrini R. Efficacy and safety of ketamine in refractory status epilepticus in children. Neurology [Internet]. Neurology; 2012 Dec 11;79(24):2355–2358. Available from: https://pubmed.ncbi.nlm.nih.gov/23197747/
- Rosati A, L’Erario M, Bianchi N, Olivotto S, Battaglia D, Darra F, Biban P, Biggeri A, Catelan D, Danieli G, Mondardini MC, Cordelli DM, Amigoni A, Cesaroni E, Conio A, Costa P, Lombardini M, Meleleo R, Pugi A, Tornaboni EE, Santarone ME, Vittorini R, Sartori S, Marini C, Vigevano F, Mastrangelo M, Pulitano SMM, Izzo F, Fusco L. KETASER01 protocol: What went right and what went wrong. Epilepsia open. 2022 Jul 14;7(3):532–540.
- Jacobwitz M, Mulvihill C, Kaufman M, Gonzalez AK, Resendiz K, MacDonald JM, Francoeur C, Helbig I, Topjian AA, Abend NS. Ketamine for Management of Neonatal and Pediatric Refractory Status Epilepticus. Neurology. 2022 Jul 11;99:e1227–e1238.
- Ilvento L, Rosati A, Marini C, L’Erario M, Mirabile L, Guerrini R. Ketamine in refractory convulsive status epilepticus in children avoids endotracheal intubation. Epilepsy & Behavior [Internet]. Academic Press; 2015 Aug 1;49:343–346. Available from: https://moh-it.pure.elsevier.com/en/publications/ketamine-in-refractory-convulsive-status-epilepticus-in-children-