Don’t Be Afraid of the Dark: Neurocritical Care Pharmacy at Night
Published on: March 17, 2023

Healthcare workers face unique challenges during evening and overnight hours: an abundance of unplanned intensive care unit (ICU) admissions, unforeseen patient decompensation, and critical treatment decisions.1 The majority of overnight neurocritical care (NCC) teams consist of one or two providers, often a resident or advanced practice provider. These providers have fewer resources, less accessibility to consult services, and indirect supervision from senior providers. Other services are also scaled back and frequently consist of less experienced team members on-site, including limited or no access to a clinical pharmacist. Add to that chronic sleep deprivation, which can impair cognitive function2, and it is clear to see how most medication errors occur during these hours.
A study conducted in critical care units found the rate of medication errors to be 16.7% during day shift (8 am – 2 pm) vs. 42.7% during evening shift (2 – 8 pm) and 28.7% during night shift (8 pm – 8 am).3 One way to combat the increase in medication errors seen on evening and overnight hours is to increase access to a clinical pharmacist. The addition of a neurocritical care-trained clinical pharmacist on all shifts would allow real time identification and correction of medication errors before they occur. In fact, the Neurocritical Care Society recommends that in addition to a dedicated clinical pharmacist, neurocritical care units should have 24-hour on call clinical pharmacy support. Furthermore, they recommend that this clinical pharmacist should have additional training in both critical care and neuropharmacology beyond what a typical clinical pharmacist may possess.4 Specialty training allows the pharmacist to be well versed in the unique challenges and complex medications of this specialized population, resulting in interventions above and beyond the low hanging fruit.
Beyond an increase in medication errors, evening and overnight shifts pose other unique challenges that a neurology-trained clinical pharmacist can help mitigate. Obtaining medication records can be quite difficult on these shifts due to limited hours of outpatient facilities and minimal access to family members. A clinical pharmacist is skilled at finding alternative avenues to obtain outpatient medication records. Additionally, they can provide 24-hour monitoring of medications with narrow therapeutic indices such as antiepileptics, antibiotics, and barbiturates. Real-time dose alterations and recommendations as a result of this monitoring can impact the duration of stay for neurologically ill patients. The additional pharmacologic support also allows providers to focus on the bigger picture within patient care and can alleviate some of the increased workload NCC providers face at night.
Our hospital provides 24-hour clinical pharmacy support on evenings and overnights to address some of the many challenges that providers face “after-hours.” Our ICU and emergency department (ED) pharmacists on evening shift are heavily integrated into the NCC team. We would like to share our practice model with examples of pharmacy-related challenges and successes.
Emergency Department (ED) After Dark: Jessie Lipstreuer
My name is Jessie, and I am one of two evening shift ED pharmacists for a Level I Trauma Center, Comprehensive Stroke Center and referral center for 21 surrounding counties. I work seven-on/seven-off from 3 pm to 1 am as the sole ED pharmacist. This schedule provides continuity of critical care coverage for our providers and patients, but it is not without challenges from a pharmacist’s perspective. There is no ED pharmacist overlap, so I start my day by receiving hand off from dayshift regarding critically ill patients within the department, as well as any incoming alerts. Operating during atypical business hours means that primary care offices and urgent cares are closed, which leads to increased ED volume and heavy utilization of ED pharmacy services. With the lack of available information, I utilize my critical thinking to provide more creative medication solutions. In addition, I am routinely in contact with our critical care pharmacist regarding patients being admitted to the ICU, providing updates, differential diagnoses, and recommendations that have not yet been addressed.
As medication experts, ED pharmacists can assist with medication selection for status epilepticus, identification of contraindications to thrombolytic therapy in acute ischemic stroke, anticoagulation reversal in intracranial hemorrhages (ICH), and intubation or resuscitation if necessary. In one recent example in my role as the ED evening pharmacist, I responded to a code stroke with the evening shift nurse practitioner for a transfer patient that had received alteplase at an outside hospital. The patient experienced an acute decline in mentation during transport and required immediate intubation upon arrival. Due to concern for potential hemorrhagic conversion, I facilitated the rapid ordering and bedside delivery of fibrinolytic reversal with aminocaproic acid and then initiated our code stroke red process once imaging confirmed an acute ICH. My involvement shortened the time it would have normally taken on evening shift for a patient to receive reversal medication and likely improved patient care.
Neurocritical Care After Dark: Brittny Medenwald
My name is Brittny, I am a PGY-2 neurocritical care-trained, critical care pharmacist. I cover the NCC unit and trauma surgical ICU on evening shift. I also work seven-on/seven-off, however, my hours are from noon until 10 pm. We follow an integrated pharmacy practice model, so I start my shift by providing order entry cross coverage for the dayshift pharmacists. Around 15:00, I receive sign out (a verbal pass-off from the day shift pharmacist) on any medication levels, acute medication issues, or critical patients that need follow up. As I cover multiple ICUs, there are no formal multidisciplinary patient rounds or sign out rounds. Instead, I try to be present when the providers pass off to their overnight counterparts to gain more insight into any patient care changes that occurred on day shift and address any medication-related issues I have come across. Since I respond to inpatient codes and provide back up for the ED pharmacist, I am not always able to attend provider hand offs, making it extremely difficult to know all the patients in as much detail as I would like. My role as the evening critical care pharmacist is to provide support and try to bridge the gap between dayshift and evening shift with respect to the medication therapy that is ordered for patients.
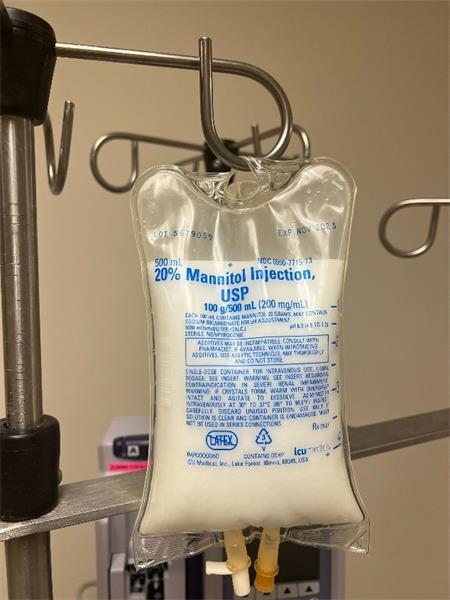
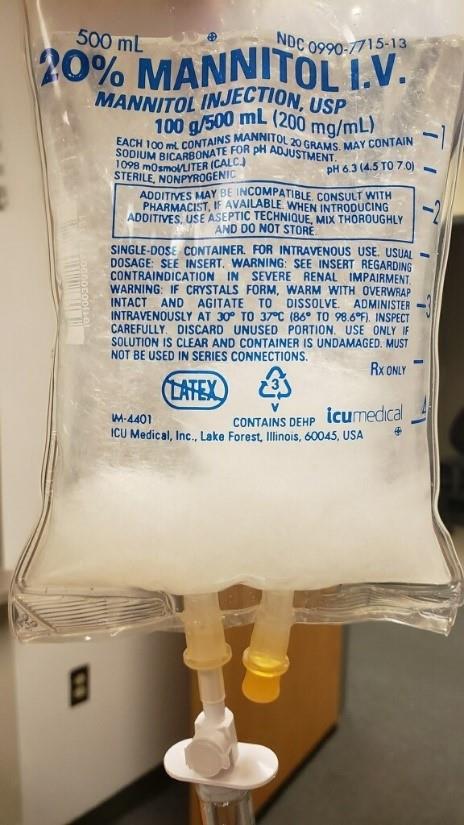
I make myself available to the nursing staff as much as possible and often rely on them for pertinent patient updates. In return, I am often able to provide additional insight on the course of a patient’s care in the ED prior to their arrival in the NCC unit as I am in frequent communication with the ED pharmacist. Once the patient arrives, most of my focus and communication is geared toward emergent problems or new issues identified during order verification. The rest of my shift is spent assisting the team in stabilizing new ICU admissions, responding to patients who are decompensating, and following up on the status of critical patients signed out by day shift ICU pharmacists. For example, one evening I noticed a milky bag of fluid hanging on the bedside of an NCC patient who was waiting for a computed tomography (CT) scan. Upon closer inspection, I realized it was a bag of completely crystalized mannitol that was primed and attached to the patient. Mannitol has a propensity for crystallizing at cooler temperatures and sometimes at room temperature (Figure 1). After ensuring the medication was not yet infusing, I provided nursing education, and expedited a replacement bag of uncrystallized mannitol. This error, and others like it, may not have been caught without the physical presence of a clinical pharmacist on the evening shift. At the end of my shift, I sign out to the overnight pharmacist.
Figure 1. Crystallized Mannitol
In addition to supporting overnight providers, a NCC pharmacist can also serve as a resource for other evening/night shift pharmacists who may encounter neurology-related issues on non-critically ill patients. With the rapid increase in the approval of monocolonal antibodies for multiple sclerosis, migraine headache, Parkinson’s and Alzheimer’s disease, patients with these medications are frequently admitted outside of the ICU. Many of these medications are parenteral with unique dosing criteria, adverse effects, and access barriers. In addition, customization of dual antiplatelet therapy is becoming increasingly common. A neurology-trained pharmacist can serve as a resource to the other evening shift pharmacists who may not be as familiar with these medications.
With the exponentially growing pool of neurology literature, a neurology-trained pharmacist has a more thorough understanding of complex neurology topics than a pharmacist with training in a different specialty. This is important because, as anyone who practices in neurology and neurocritical care can tell you, neurology is not black and white. A pharmacist needs to develop the necessary skills and expertise to provide optimal patient care in the “gray areas.”
Are You Still Afraid of the Dark?
The Standards for Neurologic Critical Care Units from the Neurocritical Care Society state that pharmacists are an essential member of the interdisciplinary care team, citing their ability to reduce medication-related costs, decrease ICU length of stay, reduce readmission rates, decrease adverse medication reactions/interactions and more. They recommend that in addition to a highly trained and dedicated pharmacist, the NCC unit should have access to 24-hour, on-call clinical pharmacy services.4 Our hospital amplifies the recommendation by providing a pharmacist in the ED with advanced training and a neurology-trained critical care pharmacist in the ICU to support our providers and decrease medication errors.
Literature shows that medication errors more than double during the evening and overnight hours.3 The examples we describe are evidence that access to a neurology-trained pharmacist on these shifts can reduce medication errors and prevent serious errors that might not have been caught otherwise due to reduced staffing and increased workload. In addition to preventing medication errors, our skill set was utilized to provide therapeutic alternatives during drug shortages, most recently for the recent national shortage of 3% saline, 23.4% saline, and mannitol. Overall this service takes some of the workload off other overnight providers while enhancing patient safety.
Twenty-four-hour clinical pharmacy support for neurocritical care patients, while not without its own challenges, is a luxury that benefits a hospital system in multiple ways. From increasing neuropharmacologic resources for providers to preventing medication errors, ED and ICU clinical pharmacists with expertise in the care of NCC patients can be beacons of light in the dark.
References
1. Roepke R, Ranzani O. Making Decisions During ICU Night Shifts: Challenges and Considerations. ICU Management & Practice [Internet]. 2020 [cited 2022 Feb10];20(2):[about 3 p.].
2. Maltese F, Adda M, Bablon A, Hraeich S, Guervilly C, Lehingue S, Wiramus S, Leone M, Martin C, Vialet R, Thirion X, Roch A, Forel JM, Papazian L. Night shift decreases cognitive performance of ICU physicians. Intensive Care Med. 2016 Mar;42(3):393-400. doi: 10.1007/s00134-015-4115-4. Epub 2015 Nov 10. PMID: 26556616.
3. Eltaybani S, Mohamed N, Abdelwareth M. Nature of nursing errors and their contributing factors in intensive care units. Nurs Crit Care. 2019 Jan;24(1):47-54. doi: 10.1111/nicc.12350. Epub 2018 Apr 27. PMID: 29701274.
4. Moheet, A.M., Livesay, S.L., Abdelhak, T. et al. Standards for Neurologic Critical Care Units: A Statement for Healthcare Professionals from The Neurocritical Care Society. Neurocrit Care 29, 145–160 (2018).