Development of a Multidisciplinary Pediatric Neurocritical Care Simulation-Based Training Curriculum in Africa
Published on: October 18, 2023
Written by Jennifer C. Munoz Pareja, MD1; Nicole O’Brien, MD2; Ericka L. Fink, MD, MS3; Marie Nader, MD4; Renad Abu- Sawwa, Pharm-D5; Dennis Simon, MD3; Hans-Joerg Lang, MD, Ph.D.6; Michael Canarie, MD4; John Appiah, MD7; Jo M Wilmshurst, MD8
Introduction
Pediatric neurological disorders contribute substantially to child mortality and years lived with disability.1,2 Lower-resourced settings in Asia and Africa bear the greatest burden globally due to a lack of trained personnel and inadequate systems of care.1,3 Improvement in equitable child outcomes requires substantial coordinated efforts to deliver high-quality clinical care across various settings (e.g., emergency services, hospital, rehabilitation), including multidisciplinary education and training efforts and optimizing triage, availability of essential equipment, and transfer to higher levels of care.4,5 A survey in 2010 identified only 148 child neurology physicians in Africa, serving a population of 927 million.6 Specialized training in child neurology in Africa remains scarce and concentrated in only a few centers. In addition, the scarcity of specialized training programs in pediatric critical care medicine (PCCM) contributes to the shortage of pediatric intensivists, nurses, and other clinicians necessary for the optimal care of critically ill children in low-resource settings, including those with neurocritical illness.7 On average, the majority of African countries have only one PICU facility, while some major cities in South Africa have pediatric intensive care units or PICUs and training programs with the capacity to provide contemporary neurocritical care and associated research, particularly after neurotrauma.8 In the absence of specialized pediatric expertise, it is often the case that critical care access for pediatric patients relies on the availability of adult ICUs or less acute care. Consequently, healthcare professionals must often migrate to high-income regions to acquire specialized training.9 Thus, a compelling argument exists for supporting the expansion of comprehensive pediatric neurocritical care (PNCC) education and training within African centers, ideally created for and led by local clinicians to align with regional needs. Implementing robust, cost-effective, accessible, locally appropriate, and multidisciplinary educational programs may thus lead to significant improvements in PNCC, ultimately enhancing health outcomes for children with neurological illnesses.
|

Figure 1. A healthcare clinician is practicing fundamental TCD scanning techniques and interpretation methods on a healthy volunteer
|
Established Pediatric Neurocritical Care Education Programs in Africa
Currently, there are a handful of international educational collaborations in pediatric emergency medicine and PCCM throughout Africa. However, only a few of them concentrate specifically on PNCC training. One such program is the transcranial Doppler (TCD) Academy led by Dr. Nicole O'Brien from Nationwide Children’s Hospital, with the objective of enhancing neurodiagnostics and neuromonitoring in sub-Saharan Africa by teaching African healthcare practitioners fundamental scanning techniques and interpretation methods for TCD. The program utilizes TCD ultrasound as a portable, non-invasive, and cost-effective tool to diagnose and monitor several neurological diseases, including stroke, sickle cell disease, cerebral malaria, and meningitis. To date, more than 40 clinicians from six centers in the Democratic Republic of the Congo, Zambia, and Malawi have completed TCD training and implemented TCD examinations in the care of neurocritically ill children (Fig 1).
Another important initiative is the Pediatric Critical Care in Resource-Limited Settings (PCCiRLS) group, which strives to enhance the treatment of critically ill children by fostering multidisciplinary education, partnerships, and collaborations worldwide, including in Africa. This international collaborative conducts a series of pre-recorded lectures on neurological and non-neurological topics, paired with virtual live case discussions to supplement and reinforce didactics. Furthermore, an impactful initiative was launched in Accra, Ghana, focused on PCCM nursing education that incorporates virtual patient case simulation via the Virtual Resus Room (VRR) (Fig 2).10 In addition, it is crucial to acknowledge the significant contributions made by Pediatric Emergency and Critical Care-Kenya (PECC-Kenya). This international partnership between the University of Nairobi and the University of Washington has been instrumental in advancing pediatric emergency medicine and PCCM through a collaborative fellowship program in Kenya. Notably, PECC-Kenya has made substantial strides in education and has effectively demonstrated the value of virtual simulation in this field.11 This venture’s approach is scalable and has the potential to significantly advance comprehensive, multidisciplinary PNCC education in Africa.
|

Figure 2. The layout of the Virtual Resus room. An open-access online simulation platform that has been used worldwide to facilitate simulation in remote settings
|
Next, the Pediatric Neurocritical Care Education Series is a bi-monthly webinar developed by members of the Pediatric Neurocritical Care Research Group (PNCRG) Subcommittee on Education.12 This live lecture series utilizes a freely accessible video platform that has been attended by 102 participants from African countries (Fig 3). The series includes four types of sessions: topical lecture, case-based panel discussion, skills lab, and journal club. The content of each session is tailored to the level of a pediatric neurocritical care trainee and is relevant to various disciplines. Topics covered to date include post-cardiac arrest care, traumatic brain injury, central nervous system infections, continuous electroencephalogram monitoring, and neurocritical care in low and middle-income countries. All sessions are recorded and posted to an online video platform for subsequent viewing. These initiatives offer excellent inclusive learning and networking opportunities for clinicians in low-resource regions (Fig 3).
|
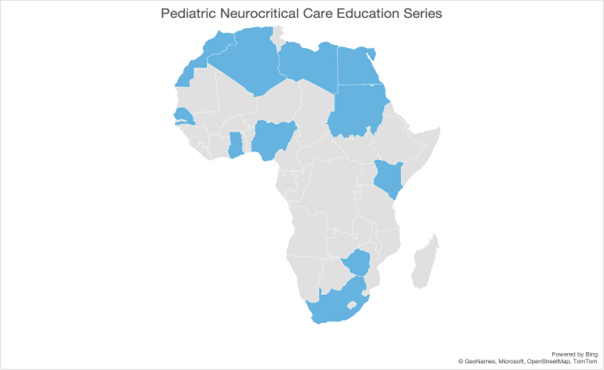
Figure 3. Countries (shaded blue) from which healthcare personnel have registered for at least one session of the Pediatric Neurocritical Care Education Series
|
Despite the sessions being free and accessible to anyone, the group has encountered several challenges. For example, there may be a segment of the population that remains unaware of these sessions despite utilizing social media and an email distribution list. Additionally, there may be language barrier-related issues, as all sessions are conducted in English without any captions or other forms of translation, posing a challenge for individuals who may not be proficient in English. Finally, some individuals may not have sufficient internet access or bandwidth to stream the sessions effectively.
To address these challenges, the group is actively exploring potential solutions to increase awareness, such as expanding its reach via different social media channels and professional society email distribution lists. Additionally, efforts are underway to provide language support tools such as captions or translations to make the sessions more inclusive. Finally, alternative means of content delivery are being explored to ensure accessibility for individuals with limited internet access or bandwidth.
Finally, it is crucial to acknowledge the remarkable and sustained efforts of various non-governmental organizations (NGOs) and academic institutions dedicated to education and sustainability in low-resource settings. These entities play a significant role in providing practical on-the-job training, often in challenging conditions, with the aim of improving access to essential critical care services. Examples of such organizations include Médecins Sans Frontières (MSF), the Alliance for International Medical Action (ALIMA), and various hospital partnerships. Programs such as Emergency Triage Assessment and Treatment (ETAT)13 are specifically designed to stabilize the ABCs (Airway, Breathing, Circulation) and provide essential care for neurological emergencies, setting the stage for more advanced curriculums. In addition, important neurological educational initiatives have been undertaken by the World Federation of Neurosurgical Societies (WFNS) and the Foundation for International Education in Neurological Surgery (FIENS).14-16
A New Pediatric Neurocritical Care Curriculum for Equitable Access to Education in Low Resource Settings
Simulation training is a vital component of skills development and learning, particularly in healthcare. Its immersive and controlled environment allows learners to practice their skills actively and apply theoretical knowledge to real-life situations. Simulation bridges the gap between theory and practice, fostering critical thinking and problem-solving abilities. It offers a safe space for learners to make mistakes and receive immediate feedback for improvement. Moreover, simulation training promotes interprofessional collaboration and teamwork, which is essential in healthcare settings. Advocacy is crucial to integrating simulation training into healthcare education, emphasizing its benefits and ensuring necessary resources and infrastructure. Customizable to different expertise levels, simulation training continues to enhance learning experiences, critical skills, and, ultimately, patient care.
Based on these premises and with the aim of promoting empowerment and sustainability within the local African healthcare community, our multidisciplinary team has assembled a diverse team of experts specializing in PNCC and simulation. Our primary goal is to develop a PNCC curriculum in partnership with multidisciplinary healthcare professionals in resource-limited settings. By collaborating closely with local clinicians, we intend to create an innovative curriculum tailored to a site’s specific resources and needs. The expectation is that this curriculum will more fully equip healthcare clinicians with the vital knowledge, skills, and tools required for effective acute care management of pediatric patients with neurocritical conditions (Fig 4,5).
|
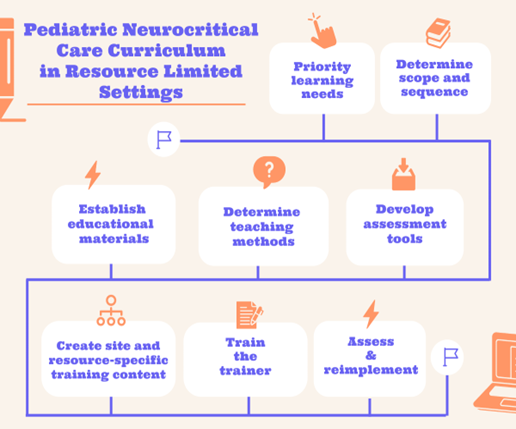
Figure 4. Roadmap to the development of a Pediatric Neurocritical Care Curriculum for resource-limited settings
|
|
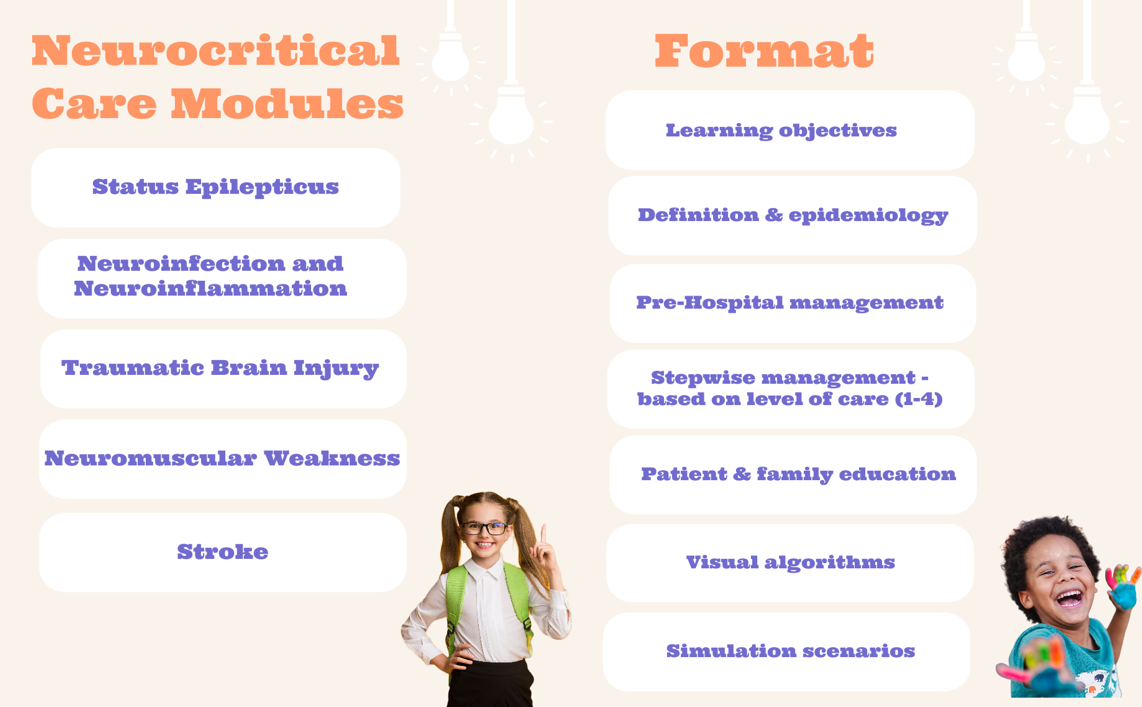
Figure 5. Highly valued topical teaching modules identified during a learning needs assessment and format for module delivery
|
This curriculum will be adaptable and tailored to the specific level of care that each patient may require, ranging from 1 to 4, according to the WHO criteria, with 4 representing the highest level of care. Specifically, this curriculum will include pre-hospital and triage management and separate treatment pathways for acute care in facilities with and without ICU availability. The curriculum is designed to be scalable and versatile, ensuring that it can effectively meet the needs of patients at different stages of their treatment journey. In addition, the simulation component will be available through a virtual platform as well as an in-person format.
Further, the curriculum is structured to align with a site’s resource status. By accounting for the context and resources of each healthcare setting, the curriculum ensures that healthcare professionals are equipped with the necessary knowledge, skills, and tools to deliver quality care in their situation. It provides them with practical guidance and strategies that can be implemented within their specific resource constraints, promoting efficient and effective patient management.
Through this adaptable and resource-conscious curriculum, we aim to promote sustainable and effective healthcare practices that can be implemented across resource-limited healthcare settings, ultimately improving outcomes for children with neurological conditions.
Conclusions and Future Directions
We aim to establish a sustainable collaboration network that transcends geographical and economic boundaries. We commend initiatives with similar missions and seek to enhance pediatric neurocritical outcomes through collaborative, multidisciplinary educational ventures that expand PNCC expertise and lead to improved access to high-quality care and outcomes. For potential collaborations with the authors and other organizations in Africa please see Appendix A.
We believe that by expanding the reach of PNCC expertise and fostering ongoing partnerships, we can make a significant and lasting impact on the care and outcomes of children with neurological conditions worldwide.
Acknowledgments
- Jenny C. Erklauer, Department of Pediatrics, Division of Pediatric Critical Care Medicine, Texas Children's Hospital, Baylor College of Medicine, Houston, TX, USA
- Nicolas Chiriboga, Department of Pediatrics, Ann & Robert H. Lurie Children's Hospital of Chicago and Northwestern University Feinberg School of Medicine, Chicago, IL, USA
- Rebecca Silvers, Division of Neurosurgery, UCSF Benioff Children's Hospital Oakland, California, USA
- Amelie von Saint Andre-von Arnim, Department of Paediatrics & Child Health, University of Nairobi, Kenyatta Hospital, Nairobi, Kenya, USA
- Brandon McLaughlin, Department of Critical Care Medicine, UPMC Children's Hospital of Pittsburgh, Pittsburgh, PA, USA
| Name |
Organization |
Contact |
| Jennifer C. Munoz Pareja, MD |
University of Miami, PNCRG |
Jcm457@med.miami.edu |
| Nicole O'Brien, MD |
The Ohio State University, PNCRG, TCD Academy |
nicole.o'brien@nationwidechildrens.org |
| Ericka Fink, MD |
University of Pittsburgh, PNCRG |
finkel@ccm.upmc.edu |
| Maria Nader, MD |
Yale University, Virtual Simulations in Ghana Project |
marie.nader@yale.edu |
| Renad Abu-Sawwa, PharmD |
University of Florida, Pediatric Neurocritical Care Pharmacist |
rabusawwarx@gmail.com |
| Dennis Simon, MD |
University of Pittsburgh, PNCRG, PNCC Lecture Series |
dennis.simon2@chp.edu |
| Hans-Joerg Lang, MD, PhD |
ALIMA, Dakar; Heidelberg Institute of Global Health; Heidelberg |
hansjoerg.lang@alima.ngo |
| Michael Canarie, MD |
Yale University, PCCiRLS |
michael.canarie@yale.edu |
| John Appiah, MD |
Komfo Anokye Hospita; Kumasi, Ghana |
adabiea@gmail.com |
| Jo M Wilmshurst, MD |
University of Cape Town, Cape Town, South Africa |
jo.wilmshurst@uct.ac.za |
| Amelie von Saint Andre-von Arnim |
University of Washington, PECC-Kenya |
ameliev@uw.edu |
References
1. Newton CR. Global Burden of Pediatric Neurological Disorders. Semin Pediatr Neurol. 2018 Oct;27:10-15. doi: 10.1016/j.spen.2018.03.002. Epub 2018 Jun 20. PMID: 30293585; PMCID: PMC7613506.
2. Childhood Acute Illness and Nutrition (CHAIN) Network. Childhood mortality during and after acute illness in Africa and south Asia: a prospective cohort study. Lancet Glob Health. 2022 May;10(5):e673-e684. doi: 10.1016/S2214-109X(22)00118-8. PMID: 35427524; PMCID: PMC9023747.
3. Fink EL, von Saint Andre-von Arnim A, Kumar R, Wilson PT, Bacha T, Aklilu AT, Teklemariam TL, Hooli S, Tuyisenge L, Otupiri E, Fabio A, Gianakas J, Kochanek PM, Angus DC, Tasker RC; Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network, PALISI Global Health Subgroup, and Prevalence of Acute Critical Neurological Disease in Children: A Global Epidemiological Assessment (PANGEA) Investigators. Traumatic Brain Injury and Infectious Encephalopathy in Children From Four Resource-Limited Settings in Africa. Pediatr Crit Care Med. 2018 Jul;19(7):649-657. doi: 10.1097/PCC.0000000000001554. PMID: 29664874.
4. World Health Organization. Emergency Triage Assessment and Treatment (ETAT): Manual for Participants. World Health Organization. https://www.who.int/publications/i/item/9241546875. Published date, February 20, 2005. Accessed [June 27, 2023].
5. United Nations. Sustainable Development Goals. United Nations Sustainable Development Goals. https://sdgs.un.org/goals. Published date, 2015. Accessed [June 27, 2023].
6. Wilmshurst JM, Badoe E, Wammanda RD, Mallewa M, Kakooza-Mwesige A, Venter A, Newton CR. Child neurology services in Africa. J Child Neurol. 2011 Dec;26(12):1555-63. doi: 10.1177/0883073811420601. Epub 2011 Oct 21. PMID: 22019842; PMCID: PMC3672989.
7. Muttalib F, González-Dambrauskas S, Lee JH, Steere M, Agulnik A, Murthy S, Adhikari NKJ; PALISI Global Health Subgroup of the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI). Pediatric Emergency and Critical Care Resources and Infrastructure in Resource-Limited Settings: A Multicountry Survey. Crit Care Med. 2021 Apr 1;49(4):671-681. doi: 10.1097/CCM.0000000000004769. PMID: 33337665.
8. Figaji AA, Graham Fieggen A, Mankahla N, Enslin N, Rohlwink UK. Targeted treatment in severe traumatic brain injury in the age of precision medicine. Childs Nerv Syst. 2017 Oct;33(10):1651-1661. doi: 10.1007/s00381-017-3562-3. Epub 2017 Aug 14. PMID: 28808845.
9. Wilmshurst J. Paediatric neurology in Africa: filling the gap. Dev Med Child Neurol. 2017 Feb;59(2):113. doi: 10.1111/dmcn.13308. PMID: 28044318.
10. Foohey S, Nagji A, Yilmaz Y, Sibbald M, Monteiro S, Chan TM. Developing the Virtual Resus Room: Fidelity, Usability, Acceptability, and Applicability of a Virtual Simulation for Teaching and Learning. Acad Med. 2022 May 1;97(5):679-683. doi: 10.1097/ACM.0000000000004364. Epub 2022 Apr 27. PMID: 34380940.
11. Maloney CE, Burns R, Hartford E, von Saint Andre-von Arnim A, Foohey S, Kailemia M, Reel B, Thomas A. International Pediatric Emergency Medicine and Critical Care Fellow Education: Utilizing Virtual Resuscitation Simulation in Settings With Differing Resources. Cureus. 2022 Feb 7;14(2):e21991. doi: 10.7759/cureus.21991. PMID: 35282505; PMCID: PMC8906565.
12. Erklauer JC, Thomas AX, Hong SJ, Appavu BL, Carpenter JL, Chiriboga-Salazar NR, Ferrazzano PA, Goldstein Z, Griffith JL, Guilliams KP, Kirschen MP, Lidsky K, Lovett ME, McLaughlin B, Munoz Pareja JC, Murphy S, O'Donnell W, Riviello JJ, Schober ME, Topjian AA, Wainwright MS, Simon DW, Pediatric Neurocritical Care Research Group. A Virtual Community of Practice: An International Educational Series in Pediatric Neurocritical Care. Children (Basel). 2022 Jul 20;9(7):1086. doi: 10.3390/children9071086. PMID: 35884070; PMCID: PMC9316633.
13. Galatsch M, Lang HJ, Noa C, Raveloharimino H, Robinson A, Rabesandratana N, Magera LI, Weigel R, Köcher-Andrianarimanana D. A mixed-methods study on evaluating an updated, francophone version of ETAT+ training in Madagascar. South Afr J Crit Care. 2022 Aug 5;38(2):10.7196/SAJCC.2022.v38i2.535. doi: 10.7196/SAJCC.2022.v38i2.535. PMID: 36284927; PMCID: PMC9549591.
14. Rallo MS, Strong MJ, Teton ZE, Muraszko K, Nanda A, Liau L, Rosseau G. Targeted Public Health Training for Neurosurgeons: An Essential Task for the Prioritization of Neurosurgery in the Evolving Global Health Landscape. Neurosurgery. 2023 Jan 1;92(1):10-17. doi: 10.1227/neu.0000000000002169. Epub 2022 Oct 25. Erratum in: Neurosurgery. 2023 Apr 1;92(4):e96. PMID: 36519856.
15. Dempsey RJ, Buckley NA. Education-based Solutions to the Global Burden of Neurosurgical Disease. World Neurosurgery, Volume 140, 2020, Pages e1-e6, ISSN 1878-8750, https://doi.org/10.1016/j.wneu.2020.01.057.
16. Lartigue JW, Dada OE, Haq M, Rapaport S, Sebopelo LA, Ooi SZY, Senyuy WP, Sarpong K, Vital A, Khan T, Karekezi C, Park KB. Emphasizing the Role of Neurosurgery Within Global Health and National Health Systems: A Call to Action. Front Surg. 2021 Oct 11;8:690735. doi: 10.3389/fsurg.2021.690735. PMID: 34708069; PMCID: PMC8542676.
Author Affiliations
1. Department of Pediatric Critical Care, Holtz Children’s Hospital, University of Miami, Miami, FL, USA
2. Department of Pediatrics, Division of Critical Care Medicine, Nationwide Children’s Hospital/The Ohio State University, Cleveland, OH, USA
3. Department of Critical Care Medicine, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
4. Department of Pediatrics, Section of Pediatric Critical Care, Yale University School of Medicine, New Haven, CT, USA
5. Department of Pediatric Neurology, College of Pharmacy, University of Florida, Gainesville, FL, USA
6. Alliance for International Medical Action (ALIMA), Dakar; Heidelberg Institute of Global Health; Heidelberg, Germany
7. Department of Pediatric Emergency Medicine, Komfo Anokye Hospital; Kumasi, Ghana
8. Department of Paediatric Neurology / African Paediatric Fellowship Program, University of Cape Town, Cape Town, South Africa