Business of Neurocritical Care: Billing Under the Attending Physician or APP—Which One is Right For You?
Published on: August 15, 2025
Since January 2022, split-shared critical care billing has been allowed. Split-shared billing enables members of a group (for example, physicians and APPs in the same Neurocritical Care Division) to aggregate their critical care billing time during a calendar day and get reimbursed for the sum of their time. Although it was known that this change was coming, many systems did not anticipate the unintended consequences and complexities that would accompany it, with changes in workflows associated with aggregate billing, valuation of attending physicians and APPs, and resultant effects on compensation models.
Historically, academic medical centers have not had an attending physician in house to capture billing associated with night-time admissions/consults or critical care services. Most such centers have a cadre of APPs who work at night and provide this vital care. Less often, a single APP takes in-house call for 24 hours at a time. However, there has been substantial variability over the years in how critical care services are billed and who bills for what services.
Now that split-shared billing is allowed, each health system has to determine whether it is most advantageous to bill under the APP and reduce their reimbursement by 15% or under the physician based on their staffing and their patient census. Assuming medical necessity, the determination begins with the premise of comparing the total critical care time provided by APPs in the group during a calendar day (e.g., midnight to 11:59 PM on March 1) versus that of the attending physician(s).
To better understand this, let us begin with a simple case of a patient with convulsive status epilepticus presenting at the beginning of the dayshift. The patient would have critical care services rendered by APP #1 associated with the admission orders, H&P, etc. Later, the attending physician comes in and provides critical care services during the day in conjunction with APP #1 during multi-disciplinary rounds. In this example, critical care provided by the attending physician and APP #1 during the day shift can be further broken into 3 periods of time:
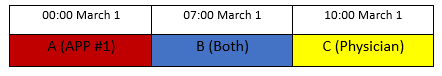
A. Time spent by APP #1 providing critical care without the attending (attributed to the APP)
Ex: Examining the patient, reviewing the electronic medical record (EMR)/medication list/labs, entering orders, documenting the critical care provided, etc.
B. Time spent by APP #1 and the attending providing critical care together (either the APP or the attending physician can claim this time, but typically claimed by the attending physician)
Ex: Attending and APP stop rounds and go into a patient’s room and treat the patient who is actively seizing with additional benzodiazepines
C. Time spent by the attending providing critical care without APP #1 (attributed to the attending)
Ex: Reviewing the MRI brain and identifying a cerebral abscess as the source of the patient’s status epilepticus, starting the patient on IV antibiotics, meeting with a family to discuss goals of care, etc.
Doing the math
If B+C are greater than A, the attending bills the cumulative time of A+B+C, and the group is eligible for 100% of charges within the constraints of the following CPT codes:
- 99291 30-74 minutes (non-CMS)
- 99291 30-103 minutes (CMS)
- 99292 each additional 30 minutes
- If B+C are less than A, the APP bills for the cumulative time of A+B+C, and the group is eligible for 85% of the charges
Night-time billing
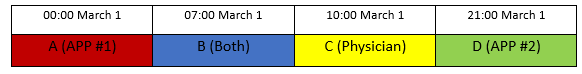
In cases where additional critical care time is provided by APP #2 after the attending has gone home, the matters are further complicated. In addition to A+B+C above, there is:
D. Time APP #2 spent providing critical care without the attending (attributed to the APP)
Ex: Titrating the patient’s benzodiazepine infusion and assessing its effect on the patient’s EEG
- In such an example it is unlikely that C or B+C will be greater than A+D or A+B+D; thus, billing would go under APP #1 for the 99291 (up to 74 or 103 minutes depending on whether it is a CMS patient or not) and APP #2 for each subsequent 99292 (at 75 minutes or greater for a non-CMS patient and 104 minutes or greater for a CMS patient), and the group would be eligible for 85% of the charges. Therefore, the attending would not submit any charge.
Now with this foundation, each organization has to look at their neurocritical care census (primary and consult patients) to determine whether billing should go under the APP(s) or under the attending physician. On average, most patients do not warrant a 99292, especially in patients with Medicare or Medicaid. However, a review of the percentage of your patients in which a 99292 is billed in comparison to the total census seen, along with use of the following Split-Shared Determination of Billing Equation (SDE) devised by the author, can help determine the optimal way for your organization to bill based on cumulative group wRVUs.
Determination of billing
n=number of patients receiving 99291 critical care billing on census
p=percentage of n in which a 99292 is billed by billing under the APP(s)
Assumptions
- wRVU (Work Relative Value Unit) 99291 = 4.5
- wRVU 99292 = 2.25
- APP billing is 85% of physician billing
- Physician billing will not lead to a 99292 due to physician not being in house at night
- Nighttime ICU coverage is provided by an APP in the same group as the attending physician
Split-Shared Determination of Billing Equation (SDE)
APP Billing = [(0.85)*(n)*(4.5)] + [(0.85)*(n)*(p)*2.25)]
Physician Billing = (4.5)*(n)
Break even occurs when APP Billing = Physician Billing
[(3.825)*(n)] + [(1.9125)*(n)*(p)] = (4.5)*(n)
(1.9125)(n)(p) = 0.675(n)
Now dividing both sides of the equation by 1.9125
(n)(p) = 0.35
Therefore, if the percentage of patients that would lead to a 99292 if billing occurred under the APP(s) but not if only billing under the single daytime attending (p) is 35%, you will break even between billing under the physician or the APP.
Examples:
If 40% of 99291 patients get a 99292 → 0.9 wRVU higher per day billing under the APP → 328.5 more wRVU annually
If 45% of 99291 patients get a 99292 → 1.85625 wRVU higher per day billing under the APP → 677.5 more wRVU annually
If 50% of 99291 patients get a 99292 → 2.8125 wRVU higher per day billing under the APP → 1026.6 more wRVU annually
Conclusions
- How to determine whether to bill under APP vs. attending physician:
- If 35% of patients receive a 99292 billing under the APP, then billing under APP(s) and billing under the physician are equivalent
- If >35% of patients receive a 99292 billing under the APP(s), then billing under APP is favored
- If <35% of patients will receive a 99292 by billing under the APP(s), then billing under physician is favored
Taking a deeper dive, you must first look at your typical daily census and determine the rounding process at your center. The key points to consider are:
-
- Does your ICU have a large number of low acuity post-operative patients who will likely just spend the night in the ICU and be transferred out in the morning (or already have transfer orders to the floor), for which you will not be able to bill for critical care?
- Is every patient seen by the attending physician or are there some patients that are seen only by the APP?
Assuming that all patients are staffed by an attending and there are very few patients for which critical care is not billed, the aforementioned SDE would apply. However, if there are many lower acuity patients (e.g., routine post-op patients and patients with floor orders), that introduces a different level of complexity, especially if not every patient is staffed by an attending. In these more complex cases, it would be best to prospectively perform these calculations for a typical non-holiday-containing month to determine what is best for your center. Thereafter, administrative leaders can use these data to best formulate the valuation and incentive processes for their physician and APP team members.