Beyond Survival: Mapping Recovery Paths After Cardiac Arrest in the POST-ICECAP Study
Published on: October 09, 2024
Introduction
Out-of-hospital cardiac arrest (OHCA) represents a critical medical emergency with high immediate mortality rates, but survival rates have improved significantly due to advances in resuscitation techniques and post-arrest care. In the United States, approximately 1,000 adults experience OHCA each day, with over 60,000 surviving to hospital discharge annually. Despite these advancements, there remains a substantial knowledge gap regarding the long-term recovery process and optimizing the continuum of care for OHCA survivors. The POST-ICECAP study aims to address this gap by investigating the long-term recovery trajectories of OHCA survivors and identifying key intervention targets to improve outcomes.
Neurocritical specialists can significantly enhance the POST-ICECAP initiative by providing expertise in neurological assessments essential for accurately evaluating cognitive impairments. They are ideally positioned to assist with patient recruitment and retention, while also incorporating rehabilitation insights to underscore the recovery potential of cardiac arrest survivors with consciousness disorders. Furthermore, these specialists can act as champions within their institutions, advocating for the outpatient needs of these survivors and fostering collaboration among healthcare providers. This teamwork can lead to the development of educational resources, ensuring a comprehensive approach to patient care.
Background
The Burden of OHCA Survivorship
Surviving an OHCA is a significant medical achievement, yet it often comes with lasting effects that can impact an individual's ability to reintegrate into their societal roles and return to work and a normal life. Survivors often face a range of challenges, including persistent neurological impairments that can impact cognitive function, functional ability, and overall health-related quality of life (HRQoL). The World Health Organization’s International Classification of Functioning, Disability, and Health (WHO-ICF) provides a framework for understanding recovery, encompassing various dimensions of physical, cognitive, and emotional health (Figure 1).
Previous studies have mainly focused on short-term outcomes within the first 1-3 months after OHCA. The lack of comprehensive long-term data has resulted in inadequate guidelines for post-discharge care and rehabilitation, underscoring the need for studies like POST-ICECAP.
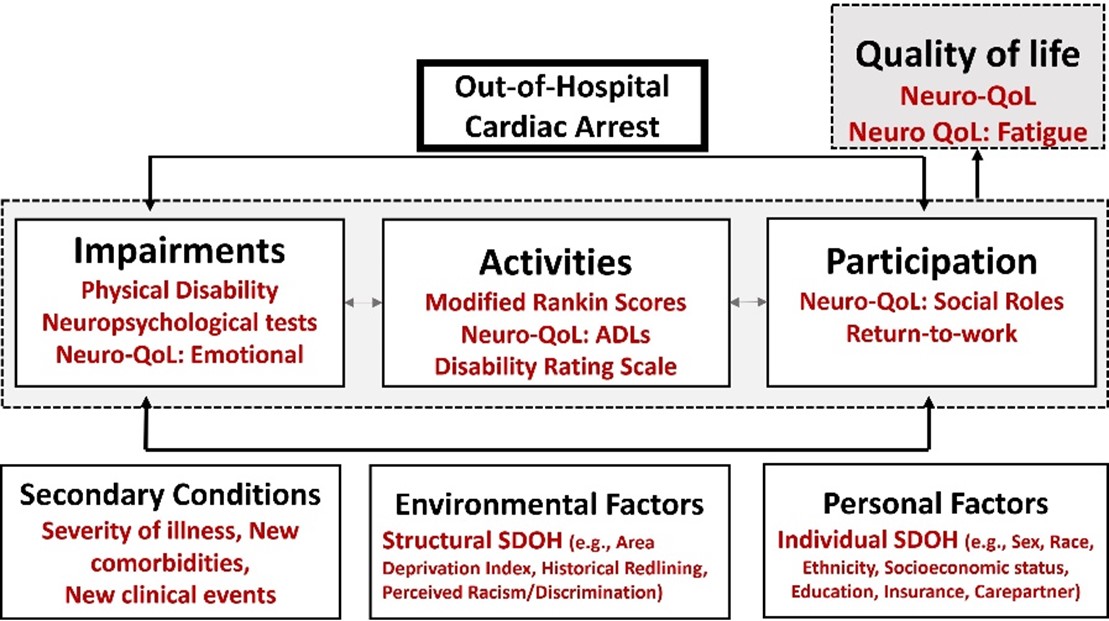
Figure 1. Proposed OHCA Recovery Framework, an adaptation of the WHO-ICF model,48 demonstrating 1) the three primary domains of recovery (impairments, activity or functional limitations, and HRQoL/participation restrictions), and 2) the influence of factors related to clinical course and individual and structural components of Social Determinants of Health (SDOH) on functional and cognitive recovery & HRQoL.
Rationale for POST-ICECAP
The POST-ICECAP study emerges as a pioneering effort to explore recovery patterns from 1 to 12 months post-OHCA. Prior research has shown significant variability in long-term outcomes, with some survivors experiencing continued improvement while others face stagnation or regression. This variability may be influenced by numerous factors, including the severity of the initial injury, the interventions received during acute care, and the intensity of post-discharge rehabilitation. Additionally, there is a critical need to understand and address disparities in recovery among different racial and ethnic groups. In Table 1, we underline the significance of POST-ICECAP in understanding survivorship and recovery after surviving OHCA. In Table 2, we further elucidate how neurocritical care specialists can significantly enhance the quality and impact of POST-ICECAP.
Study Objectives and Design
Objectives
The POST-ICECAP study is designed to achieve several key objectives (Figure 2):
1. Characterize Recovery Patterns: The study will track recovery trajectories of OHCA survivors from 1 to 12 months, focusing on functional, cognitive, and HRQoL outcomes. This will involve assessing how recovery is influenced by illness severity scores such as the Pittsburgh Cardiac Arrest Category Score, and critical care interventions including ICECAP randomized arms and early vs. late angiography received during acute care.
2. Estimate Rehabilitation Impact: The study will investigate whether acute inpatient rehabilitation, compared to outpatient therapy or no rehabilitation, is associated with improved recovery outcomes.
3. Examine Disparities in Recovery: POST-ICECAP will explore racial and ethnic disparities in recovery and identify potential mechanisms contributing to these disparities.
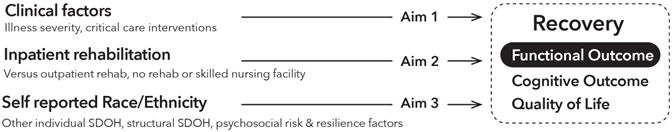
Figure 2. Study Specific Aims
Study Design
POST-ICECAP is a prospective cohort study involving patients who survive to 1-month post-OHCA. Participants will undergo detailed follow-up with in-person visits at 3 and 12 months and telephone/videoconferencing visits at 1, 6, and 9 months (Figure 3). This comprehensive approach allows for a thorough assessment of recovery over time, including functional, cognitive, and HRQoL measures.
The study, funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Heart, Lung, and Blood Institute (NHLBI), builds on the infrastructure of the Influence of Cooling Duration on Efficacy in Cardiac Arrest Patients (ICECAP) trial. The trial is being conducted within the NIH-funded Strategies to Innovate Emergency Care Clinical Trials Network (SIREN). Supported by the Neurocritical Care Society’s Curing Coma®, POST-ICECAP is currently enrolling participants and involves approximately 50 hospitals in the ICECAP trial, creating a diverse network that will facilitate a robust analysis of 1,000 OHCA survivors' recovery patterns across different settings and populations.
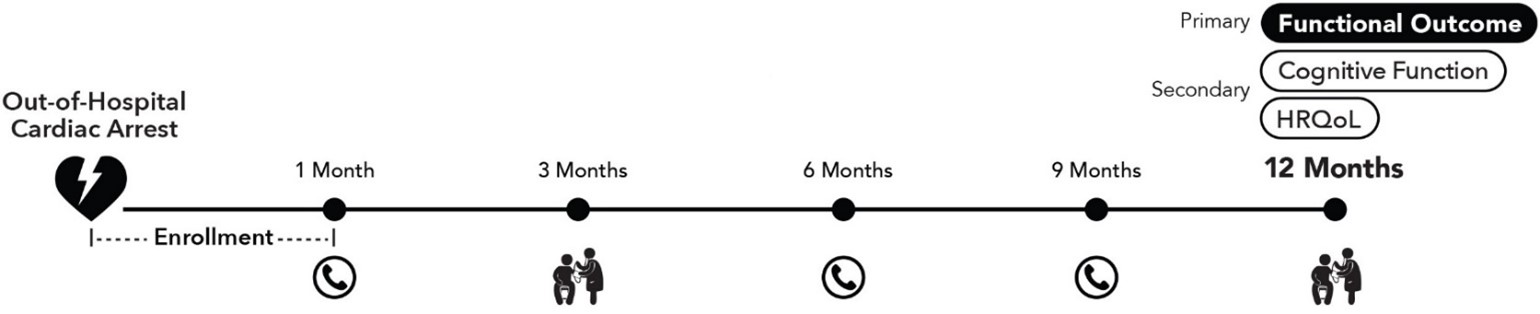
Figure 3. POST-ICECAP Study Visits
Key Measures
Study Outcomes
Trajectories of Functional Recovery
Functional outcomes will be evaluated using the Modified Rankin Scale, a well-established measure that assesses disability and dependence in daily activities. This measure is crucial for understanding how well survivors can return to their pre-arrest level of functioning or adapt to new limitations.
Cognitive Function
Cognitive recovery will be assessed using the age-adjusted standardized cognition score and summary scores from a battery of neuropsychological tests including the NIH Toolbox and Brief Test of Adult Cognition by Telephone (BTACT). This approach allows for a nuanced understanding of cognitive impairments, which are common among OHCA survivors and significantly affect their quality of life and ability to return to work.
Health-Related Quality of Life (HRQoL) and Societal Participation
HRQoL will be measured using the NIH Neuro-QoL, capturing overall well-being and the impact of health on various life domains. Societal participation will also be evaluated, as engagement in social and leisure activities is closely tied to functional recovery and overall quality of life.
Factors That May Influence Recovery in POST-ICECAP
Severity of Brain Injury Sets the Stage for Variability in Recovery
Whether long-term outcomes are associated with illness severity scores and interventions received during acute care that predict survival and functional status at hospital discharge is a knowledge gap. POST-ICECAP will leverage the comprehensive and systematically collected physiological and biomedical data to examine how these physiological assessments are associated with recovery.
Acute Rehabilitation and Social Determinants of Health May Play a Significant Role in Shaping Recovery
POST-ICECAP will explore the effects of acute inpatient rehabilitation on recovery outcomes for OHCA survivors. With no established guidelines for neurorehabilitation in this population, this aspect of the study is crucial for advancing care practices. Additionally, the study will investigate how social determinants of health—including race, ethnicity, socioeconomic factors at both individual and neighborhood levels, and experiences of discrimination—affect recovery outcomes. This comprehensive approach aims to uncover how these factors influence the recovery process and help tailor interventions to improve overall outcomes.
Psychological Distress: A Key Feature of OHCA Survivorship
The study will also assess psychological distress among OHCA survivors, focusing on prevalent issues such as post-traumatic stress disorder, depression, and anxiety. POST-ICECAP aims to document the prevalence of these psychological challenges and identify their predictors. By exploring the psychological aspects of recovery, the study will provide valuable insights into how these issues relate to functional outcomes and HRQoL over time.
OHCA Survivors with Disorders of Consciousness (DoC): A Critical But Neglected Subgroup
Withdrawal of life-sustaining treatments is common for patients with DoC—those who are unresponsive and unable to follow simple commands—within a few days of an OHCA. This practice stems from limited data on long-term recovery and a prevailing belief among clinicians that such patients are unlikely to show significant improvement. The proposed study aims to challenge this assumption by identifying patients who may still have the potential to recover. As the largest study of its kind, POST-ICECAP will systematically explore the natural clinical course of patients who remain unresponsive before hospital discharge, offering new insights into their potential for recovery.
Conclusion
The POST-ICECAP study represents a significant advancement in understanding long-term recovery after OHCA. By focusing on recovery trajectories from 1 to 12 months post-arrest, the study aims to address critical knowledge gaps and provide evidence-based insights into the factors influencing recovery. The findings from POST-ICECAP are expected to inform clinical practice, guide rehabilitation efforts, and address disparities in recovery outcomes, ultimately improving the quality of care and support for OHCA survivors. This comprehensive approach will not only enhance our understanding of recovery but also pave the way for more effective interventions and equitable care strategies for this vulnerable population.
For more information on the study, please visit POST-ICECAP Study website.
Table 1. Significance of POST-ICECAP in enhancing care and understanding the challenges faced by cardiac arrest survivors.
|
1. Understanding Neurological Impact: Cardiac arrest can lead to various neurological deficits and long-term outcomes will help in understanding the extent and progression of these deficits over time.
|
|
2. Informed Rehabilitation Strategies: Insights from long-term outcomes can guide neurocritical specialists in offering effective rehabilitation protocols tailored to the specific needs of cardiac arrest survivors.
|
|
3. Patient Prognosis and Care Planning: Data on survival rates and functional outcomes will aid specialists in making more accurate prognoses and care plans.
|
|
4. Inform interventions: Identification of targets aimed at improving the overall quality of life for survivors, addressing both physical and psychological aspects.
|
|
5. Family and Caregiver Support: Understanding long-term outcomes can also highliTable 2. Various ways neurocritical specialists can contribute to POST-ICECAP studyght the needs of family members and caregivers, leading to better support systems.
|
|
6. Guiding Policy and Protocols: Findings can influence clinical guidelines and policies, leading to improved standards of care.
|
|
7. Collaborative Care Models: Long-term studies can emphasize the importance of interdisciplinary approaches, fostering collaboration between cardiologists, neurologists, and rehabilitation specialists.
|
|
8. Advancing Innovation in Research and Education: Knowledge from POST-ICECAP will contribute to the broader field of neurocritical care research and training of healthcare professionals involved in the care of cardiac arrest survivors.
|
Table 2. Various ways neurocritical specialists can contribute to POST-ICECAP study
|
1. Expertise in Neurological Assessment: They can provide specialized knowledge in assessing neurological function and cognitive deficits, ensuring accurate evaluation of patient outcomes.
|
|
2. Patient Recruitment and Retention: They can assist in recruiting patients for the study.
|
|
3. Integration of Rehabilitation Insights: Neurocritical care specialists can highlight the recovery potential of cardiac arrest survivors with disorders of consciousness by incorporating effective rehabilitation practices.
|
|
4. Advocacy for Survivors: Neurocritical specialists can advocate for the outpatient needs of cardiac arrest survivors, ensuring that their voices are heard in research and policy discussions.
|
|
5. Collaboration with Multidisciplinary Teams: Neurocritical specialists can facilitate collaboration between various healthcare providers and help develop educational materials, ensuring a holistic, knowledgeable approach to patient care in the study.
|